Tuesday Poster Session
Category: Endoscopy Video Forum
P3887 - GOOPS! Iatrogenic Gastric Outlet Obstruction After Endoscopic Full Thickness Resection of a Duodenal NET
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shantanu Solanki, MD, MPH
MD Anderson Cancer Center
Houston, TX
Presenting Author(s)
Shantanu Solanki, MD, MPH, Jeffrey H.. Lee, MD, MPH, FACG, Phillip Ge, MD, Emmanuel Coronel, MD
MD Anderson Cancer Center, Houston, TX
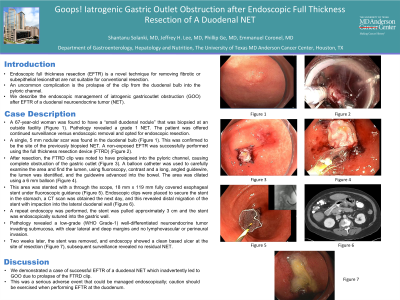
Introduction: Endoscopic full thickness resection (EFTR) is a novel technique for removing fibrotic or subepithelial lesions that are not suitable for conventional resection. An uncommon complication is the prolapse of the clip from the duodenal bulb into the pyloric channel. We describe the endoscopic management of iatrogenic gastric outlet obstruction (GOO) after EFTR of a duodenal neuroendocrine tumor (NET).
Case Description/Methods: A 67-year-old woman was found to have a “small duodenal nodule” that was biopsied at an outside facility. Pathology revealed a grade 1 NET. The patient was offered continued surveillance versus endoscopic removal and opted for endoscopic resection. A single, 5 mm nodular scar was found in the duodenal bulb. This was confirmed to be the site of the previously biopsied NET. A non-exposed EFTR was successfully performed using the full thickness resection device (FTRD). After resection, the FTRD clip was noted to have prolapsed into the pyloric channel, causing complete obstruction of the gastric outlet. A balloon catheter was used to carefully examine the area and find the lumen, using fluoroscopy, contrast and a long, angled guidewire, the lumen was identified, and the guidewire advanced into the bowel. The area was dilated using a 6 mm balloon. This area was stented with a through the scope, 18 mm x 119 mm fully covered esophageal stent under fluoroscopic guidance. Endoscopic clips were placed to secure the stent in the stomach, a CT scan was obtained the next day, and this revealed distal migration of the stent with impaction into the lateral duodenal wall. A repeat endoscopy was performed, the stent was pulled approximately 3 cm and the stent was endoscopically sutured into the gastric wall. Pathology revealed a low-grade (WHO Grade-1) well-differentiated neuroendocrine tumor invading submucosa, with clear lateral and deep margins and no lymphovascular or perineural invasion. Two weeks later, the stent was removed, and endoscopy showed a clean based ulcer at the site of resection, subsequent surveillance revealed no residual NET.
Discussion: We demonstrated a case of successful EFTR of a duodenal NET which inadvertently led to GOO due to prolapse of the FTRD clip. This was a serious adverse event that could be managed endoscopically; caution should be exercised when performing EFTR at the duodenum.
Disclosures:
Shantanu Solanki, MD, MPH, Jeffrey H.. Lee, MD, MPH, FACG, Phillip Ge, MD, Emmanuel Coronel, MD. P3887 - GOOPS! Iatrogenic Gastric Outlet Obstruction After Endoscopic Full Thickness Resection of a Duodenal NET, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
MD Anderson Cancer Center, Houston, TX
Introduction: Endoscopic full thickness resection (EFTR) is a novel technique for removing fibrotic or subepithelial lesions that are not suitable for conventional resection. An uncommon complication is the prolapse of the clip from the duodenal bulb into the pyloric channel. We describe the endoscopic management of iatrogenic gastric outlet obstruction (GOO) after EFTR of a duodenal neuroendocrine tumor (NET).
Case Description/Methods: A 67-year-old woman was found to have a “small duodenal nodule” that was biopsied at an outside facility. Pathology revealed a grade 1 NET. The patient was offered continued surveillance versus endoscopic removal and opted for endoscopic resection. A single, 5 mm nodular scar was found in the duodenal bulb. This was confirmed to be the site of the previously biopsied NET. A non-exposed EFTR was successfully performed using the full thickness resection device (FTRD). After resection, the FTRD clip was noted to have prolapsed into the pyloric channel, causing complete obstruction of the gastric outlet. A balloon catheter was used to carefully examine the area and find the lumen, using fluoroscopy, contrast and a long, angled guidewire, the lumen was identified, and the guidewire advanced into the bowel. The area was dilated using a 6 mm balloon. This area was stented with a through the scope, 18 mm x 119 mm fully covered esophageal stent under fluoroscopic guidance. Endoscopic clips were placed to secure the stent in the stomach, a CT scan was obtained the next day, and this revealed distal migration of the stent with impaction into the lateral duodenal wall. A repeat endoscopy was performed, the stent was pulled approximately 3 cm and the stent was endoscopically sutured into the gastric wall. Pathology revealed a low-grade (WHO Grade-1) well-differentiated neuroendocrine tumor invading submucosa, with clear lateral and deep margins and no lymphovascular or perineural invasion. Two weeks later, the stent was removed, and endoscopy showed a clean based ulcer at the site of resection, subsequent surveillance revealed no residual NET.
Discussion: We demonstrated a case of successful EFTR of a duodenal NET which inadvertently led to GOO due to prolapse of the FTRD clip. This was a serious adverse event that could be managed endoscopically; caution should be exercised when performing EFTR at the duodenum.
Disclosures:
Shantanu Solanki indicated no relevant financial relationships.
Jeffrey Lee: Boston Scientific – Consultant. Pentax – Consultant.
Phillip Ge: Alira Health – Consultant. Boston Scientific – Consultant. Fujifilm Medical Systems – Consultant. Neptune Medical – Consultant. Olympus America – Consultant. Ovesco Endoscopy USA – Consultant.
Emmanuel Coronel indicated no relevant financial relationships.
Shantanu Solanki, MD, MPH, Jeffrey H.. Lee, MD, MPH, FACG, Phillip Ge, MD, Emmanuel Coronel, MD. P3887 - GOOPS! Iatrogenic Gastric Outlet Obstruction After Endoscopic Full Thickness Resection of a Duodenal NET, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
