Tuesday Poster Session
Category: Endoscopy Video Forum
P3888 - Transoral Incisionless Fundoplication as Rescue Therapy for Gastroesophageal Reflux in a Lung Transplant Recipient
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
William W. King, MD
University of Florida College of Medicine
GAINESVILLE, FL
Presenting Author(s)
William King, MD, Hannah Zuercher, MD, Manuel Amaris, MD, Amir Emtiazjoo, MD, Mindaugas Rackauskas, MD, PhD, Bashar Qumseya, MD, MPH
University of Florida College of Medicine, Gainesville, FL
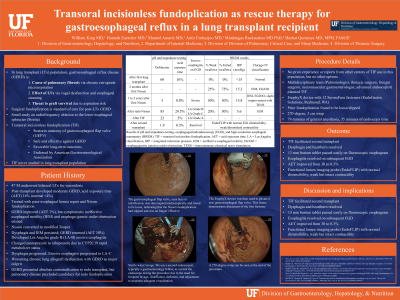
Introduction: Transoral incisionless fundoplication (TIF) is a durable and effective alternative to surgical fundoplication. It has not previously been reported in a lung transplant recipient.
Case Description/Methods: A 47-year-old man underwent bilateral lung transplant for sarcoidosis. Post-transplant acid exposure time was 16% (normal < 4%), and high-resolution esophageal manometry was normal. He underwent laparoscopic paraesophageal hernia repair with Nissen fundoplication. Although his acid exposure time improved to 1%, he developed dysphagia, ineffective esophageal motility and esophago-gastric outlet obstruction on high-resolution esophageal manometry. We therefore converted the Nissen fundoplication to a modified Toupet. Unfortunately, he developed recurrent heartburn. We switched his proton pump inhibitor to rabeprazole due to CYP2C19 ultrarapid metabolizer status, resulting in modest symptom improvement and dysphagia progression. He developed chronic lung allograft dysfunction with gastroesophageal reflux disease as a major contributor. Surveillance testing revealed acid exposure time of 30% and severe erosive esophagitis (Los Angeles grade C). The multidisciplinary lung transplant team determined that redo surgical fundoplication posed an unacceptable risk due to his declining respiratory status, and the patient strongly opposed long-term jejunal feeding. Given the lack of alternatives, the multidisciplinary lung transplant team recommended TIF as rescue therapy. During esophagogastroduodenoscopy, we found the gastroesophageal flap valve to be loose. Under general anesthesia, we used an EsophyX device to repair the existing fundoplication, creating a 270-degree, 3-cm wrap using 12 fasteners. The procedure required 79 minutes of mechanical ventilation and 35 minutes of endoscopy time. Dysphagia and heartburn resolved, and a 13mm barium tablet passed easily on fluoroscopic esophagram. Repeat esophagogastroduodenoscopy 2 months later demonstrated improvement in erosive esophagitis from Los Angeles grade C to A and a normal 270 fundoplication anatomy. Acid exposure time improved to 5%. EndoFLIP revealed normal distensibility and weak but intact contractility. With improved esophageal function, and resolution of esophageal symptoms, the risk of gastroesophageal reflux disease threatening a second lung graft was mitigated. The patient received a second lung transplant 2 months later.
Discussion: TIF may be a viable alternative to surgical fundoplication in lung transplant recipients, but further research is needed before this procedure can be incorporated into routine practice in this population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
William King, MD, Hannah Zuercher, MD, Manuel Amaris, MD, Amir Emtiazjoo, MD, Mindaugas Rackauskas, MD, PhD, Bashar Qumseya, MD, MPH. P3888 - Transoral Incisionless Fundoplication as Rescue Therapy for Gastroesophageal Reflux in a Lung Transplant Recipient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Florida College of Medicine, Gainesville, FL
Introduction: Transoral incisionless fundoplication (TIF) is a durable and effective alternative to surgical fundoplication. It has not previously been reported in a lung transplant recipient.
Case Description/Methods: A 47-year-old man underwent bilateral lung transplant for sarcoidosis. Post-transplant acid exposure time was 16% (normal < 4%), and high-resolution esophageal manometry was normal. He underwent laparoscopic paraesophageal hernia repair with Nissen fundoplication. Although his acid exposure time improved to 1%, he developed dysphagia, ineffective esophageal motility and esophago-gastric outlet obstruction on high-resolution esophageal manometry. We therefore converted the Nissen fundoplication to a modified Toupet. Unfortunately, he developed recurrent heartburn. We switched his proton pump inhibitor to rabeprazole due to CYP2C19 ultrarapid metabolizer status, resulting in modest symptom improvement and dysphagia progression. He developed chronic lung allograft dysfunction with gastroesophageal reflux disease as a major contributor. Surveillance testing revealed acid exposure time of 30% and severe erosive esophagitis (Los Angeles grade C). The multidisciplinary lung transplant team determined that redo surgical fundoplication posed an unacceptable risk due to his declining respiratory status, and the patient strongly opposed long-term jejunal feeding. Given the lack of alternatives, the multidisciplinary lung transplant team recommended TIF as rescue therapy. During esophagogastroduodenoscopy, we found the gastroesophageal flap valve to be loose. Under general anesthesia, we used an EsophyX device to repair the existing fundoplication, creating a 270-degree, 3-cm wrap using 12 fasteners. The procedure required 79 minutes of mechanical ventilation and 35 minutes of endoscopy time. Dysphagia and heartburn resolved, and a 13mm barium tablet passed easily on fluoroscopic esophagram. Repeat esophagogastroduodenoscopy 2 months later demonstrated improvement in erosive esophagitis from Los Angeles grade C to A and a normal 270 fundoplication anatomy. Acid exposure time improved to 5%. EndoFLIP revealed normal distensibility and weak but intact contractility. With improved esophageal function, and resolution of esophageal symptoms, the risk of gastroesophageal reflux disease threatening a second lung graft was mitigated. The patient received a second lung transplant 2 months later.
Discussion: TIF may be a viable alternative to surgical fundoplication in lung transplant recipients, but further research is needed before this procedure can be incorporated into routine practice in this population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
William King indicated no relevant financial relationships.
Hannah Zuercher indicated no relevant financial relationships.
Manuel Amaris indicated no relevant financial relationships.
Amir Emtiazjoo indicated no relevant financial relationships.
Mindaugas Rackauskas indicated no relevant financial relationships.
Bashar Qumseya indicated no relevant financial relationships.
William King, MD, Hannah Zuercher, MD, Manuel Amaris, MD, Amir Emtiazjoo, MD, Mindaugas Rackauskas, MD, PhD, Bashar Qumseya, MD, MPH. P3888 - Transoral Incisionless Fundoplication as Rescue Therapy for Gastroesophageal Reflux in a Lung Transplant Recipient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
