Tuesday Poster Session
Category: Endoscopy Video Forum
P3891 - Novel Technique for EUS-Guided Endoscopic Gastroenterostomy: The Dual Scope Method
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Frances Dang, MD
University of California, Irvine
Orange, CA
Presenting Author(s)
Frances Dang, MD1, Amirali Tavangar, MD1, Michael Andrew Yu, MD1, Alyssa Choi, MD2, Usman Rahim, MD3, Andrew Giap, MD, FACG4, Jason Samarasena, MD1
1University of California, Irvine, Orange, CA; 2University of Washington School of Medicine and VA Puget Sound Health Care System, Seattle, WA; 3University of California Irvine Digestive Health Institute, Exeter, CA; 4Kaiser Permanente, Irvine, CA
Introduction: Endoscopic ultrasound (EUS)-guided endoscopic gastroenterostomy has been a major advance in the management of patients with malignant gastroduodenal outlet obstruction. The most common technique is the nasobiliary drain technique, which involves advancing a nasobiliary drain over a guidewire beyond the obstruction for fluid instillation. This method has disadvantages including challenges with the catheter placement, scope exchange and fluid leaving the target bowel prematurely before puncture. In this video, we describe a novel “dual scope” technique which employs an ultra-slim gastroscope to serve as the “catheter” for water instillation of the bowel. </span>
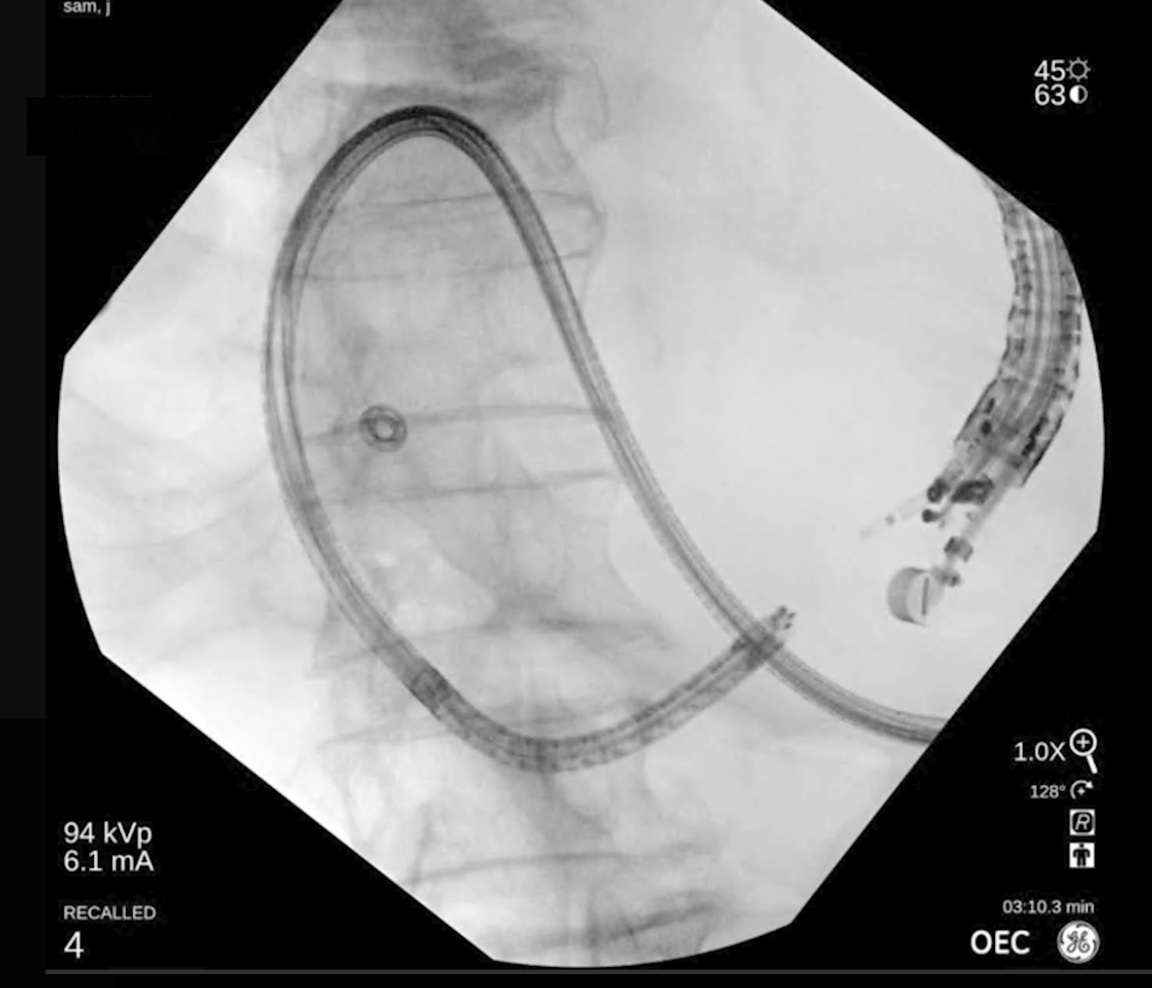
Case Description/Methods: A 55-year-old woman with metastatic gastric adenocarcinoma presented with obstruction of the pylorus from the tumor. With the dual scope method an ultra-slim gastroscope with a 2.2 mm channel first is used to traverse the obstruction. The scope is advanced as far into the duodenum as possible; Then the scope is outfitted with a water adaptor cap and will serve as the ”catheter” to instill water into the bowel lumen. The scope handle is laid down in a stable position usually on the patient or a table stand. The umbilicus is then removed from the processor and placed nearby. The therapeutic EUS scope is then advanced through the mouth alongside the ultra-slim scope. Fluoroscopy can be used to identify the tip of the ultra-slim scope and if the scope is in a desirable position in the bowel, water is instilled into the bowel using the foot pedal via the working channel of the ultra-slim gastroscope. In standard fashion, the bowel is punctured with the lumen-apposing metal stent (LAMS) system and after stent deployment, the EUS scope is removed from the mouth. The ultraslim scope is then reattached to the processor and stent inspected immediately to ensure successful fistulization with the small bowel.
Discussion: The placement of a lumen apposing metal stent to create a gastrojejunal anastomosis is a great advance in the field, but must be performed with the utmost concern for safety. With the "dual-scope" method described, we can rapidly and continuously fill the intestinal lumen via the ultra-slim scope using foot activated water jet, providing a large target for EUS-guided puncture of the bowel. Furthermore, passage of the scope past the stricture is often easier than passing a wire and nasobiliary drain. Lastly, given the ultra-slim scope is left indwelling during the procedure and serves as “the catheter”, there is no exchange needed of the scope.
Disclosures:
Frances Dang, MD1, Amirali Tavangar, MD1, Michael Andrew Yu, MD1, Alyssa Choi, MD2, Usman Rahim, MD3, Andrew Giap, MD, FACG4, Jason Samarasena, MD1. P3891 - Novel Technique for EUS-Guided Endoscopic Gastroenterostomy: The Dual Scope Method, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California, Irvine, Orange, CA; 2University of Washington School of Medicine and VA Puget Sound Health Care System, Seattle, WA; 3University of California Irvine Digestive Health Institute, Exeter, CA; 4Kaiser Permanente, Irvine, CA
Introduction: Endoscopic ultrasound (EUS)-guided endoscopic gastroenterostomy has been a major advance in the management of patients with malignant gastroduodenal outlet obstruction. The most common technique is the nasobiliary drain technique, which involves advancing a nasobiliary drain over a guidewire beyond the obstruction for fluid instillation. This method has disadvantages including challenges with the catheter placement, scope exchange and fluid leaving the target bowel prematurely before puncture. In this video, we describe a novel “dual scope” technique which employs an ultra-slim gastroscope to serve as the “catheter” for water instillation of the bowel. </span>
Case Description/Methods: A 55-year-old woman with metastatic gastric adenocarcinoma presented with obstruction of the pylorus from the tumor. With the dual scope method an ultra-slim gastroscope with a 2.2 mm channel first is used to traverse the obstruction. The scope is advanced as far into the duodenum as possible; Then the scope is outfitted with a water adaptor cap and will serve as the ”catheter” to instill water into the bowel lumen. The scope handle is laid down in a stable position usually on the patient or a table stand. The umbilicus is then removed from the processor and placed nearby. The therapeutic EUS scope is then advanced through the mouth alongside the ultra-slim scope. Fluoroscopy can be used to identify the tip of the ultra-slim scope and if the scope is in a desirable position in the bowel, water is instilled into the bowel using the foot pedal via the working channel of the ultra-slim gastroscope. In standard fashion, the bowel is punctured with the lumen-apposing metal stent (LAMS) system and after stent deployment, the EUS scope is removed from the mouth. The ultraslim scope is then reattached to the processor and stent inspected immediately to ensure successful fistulization with the small bowel.
Discussion: The placement of a lumen apposing metal stent to create a gastrojejunal anastomosis is a great advance in the field, but must be performed with the utmost concern for safety. With the "dual-scope" method described, we can rapidly and continuously fill the intestinal lumen via the ultra-slim scope using foot activated water jet, providing a large target for EUS-guided puncture of the bowel. Furthermore, passage of the scope past the stricture is often easier than passing a wire and nasobiliary drain. Lastly, given the ultra-slim scope is left indwelling during the procedure and serves as “the catheter”, there is no exchange needed of the scope.
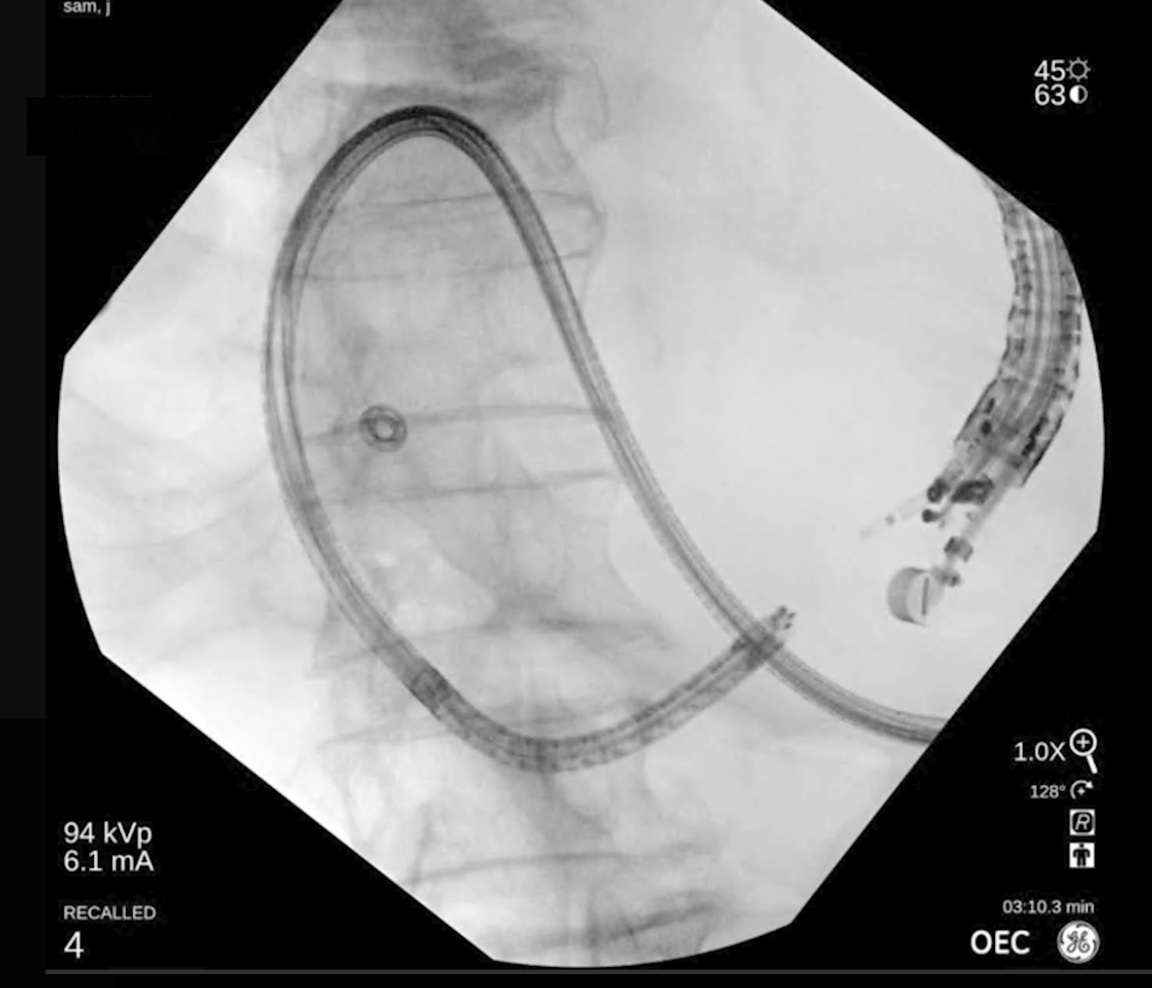
Figure: Fluroscopic image of dual scope technique to perform Endoscopic Gastrojejunostomy
Disclosures:
Frances Dang indicated no relevant financial relationships.
Amirali Tavangar indicated no relevant financial relationships.
Michael Andrew Yu indicated no relevant financial relationships.
Alyssa Choi indicated no relevant financial relationships.
Usman Rahim indicated no relevant financial relationships.
Andrew Giap indicated no relevant financial relationships.
Jason Samarasena: Cook Medical – Consultant. Medtronic – Advisory Committee/Board Member, Consultant. Neptune Medical – Advisory Committee/Board Member, Consultant. Olympus – Advisory Committee/Board Member, Consultant. Ovesco – Advisory Committee/Board Member, Consultant, Speakers Bureau. SatisfAI – Stock-privately held company. Steris – Advisory Committee/Board Member.
Frances Dang, MD1, Amirali Tavangar, MD1, Michael Andrew Yu, MD1, Alyssa Choi, MD2, Usman Rahim, MD3, Andrew Giap, MD, FACG4, Jason Samarasena, MD1. P3891 - Novel Technique for EUS-Guided Endoscopic Gastroenterostomy: The Dual Scope Method, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
