Tuesday Poster Session
Category: Endoscopy Video Forum
P3892 - EBACS (Endoscopic Bypass of Abscess With Covered Stent)
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mayank Goyal, MBBS
Mayo Clinic
Rochester, MN
Presenting Author(s)
Mayank Goyal, MBBS, Ashwariya Ohri, MBBS, Anmol Bains, MBBS, Yadwinder Singh, MBBS, Laurens Janssens, MD, Navtej Buttar, MD
Mayo Clinic, Rochester, MN
Introduction: Sleeve gastrectomy is an effective weight loss procedure technically less complex than Roux-en-Y gastric bypass. However, staple line leak (SLL) remains a significant complication of this procedure. These leaks can be associated with abscess formation. Multiple treatment strategies for SLL are reported, including surgical re-exploration, percutaneous drainage, and endoscopic stenting. Thus, we describe a novel endoscopic solution for managing post-sleeve gastrectomy stable line abscess drainage using a fully covered extra-luminal out-in-stent.
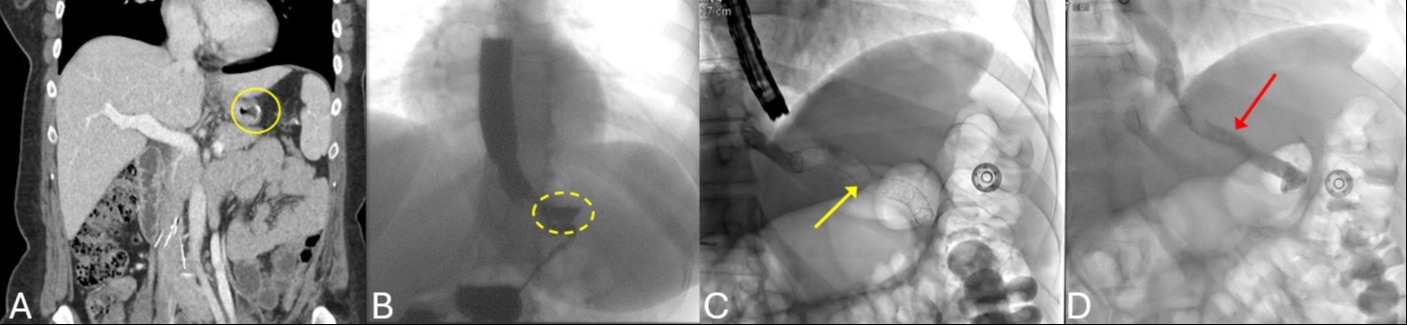
Case Description/Methods: We present the case of a 35-year-old woman with a history of gastric sleeve done two years back who presented to the emergency department with complaints of worsening abdominal pain for 3 weeks. Computed tomography abdomen showed post-surgical gastric sleeve changes with new ill-defined fluid containing cavities around the staple line, perigastric thickening, and gastrosplenic ligament edema. This was confirmed by an esophagram that also showed fluid-filled density (3.3cm) along the posterior aspect of the stomach connecting to the proximal stomach. Endoscopy revealed a disrupted sleeve gastrectomy staple line at two different areas with a larger proximal and smaller distal abscess cavity. Pus was exuding from the cavities, and both areas were irrigated. We intentionally connected the two cavities with guide wire-assisted blunt dissection. A fully covered 10x10 Viabil stent was used as an out-in-stent to bypass the abscess cavities under fluoroscopic guidance. The stent exited the sleeve, bypassed the proximal and the distal cavities, and reentered the sleeve lumen from the distal abscess cavity. The stent was secured with sutures. The patient has remained symptom-free for 3 months and the stent was removed. Fluoroscopic imaging showed no contrast extending the gastric lumen and previous fistula opening had closed.
Discussion: We show a novel management approach to manage abscess cavities at disrupted staple line using extraluminal out-in-stent.
Disclosures:
Mayank Goyal, MBBS, Ashwariya Ohri, MBBS, Anmol Bains, MBBS, Yadwinder Singh, MBBS, Laurens Janssens, MD, Navtej Buttar, MD. P3892 - EBACS (Endoscopic Bypass of Abscess With Covered Stent), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Sleeve gastrectomy is an effective weight loss procedure technically less complex than Roux-en-Y gastric bypass. However, staple line leak (SLL) remains a significant complication of this procedure. These leaks can be associated with abscess formation. Multiple treatment strategies for SLL are reported, including surgical re-exploration, percutaneous drainage, and endoscopic stenting. Thus, we describe a novel endoscopic solution for managing post-sleeve gastrectomy stable line abscess drainage using a fully covered extra-luminal out-in-stent.
Case Description/Methods: We present the case of a 35-year-old woman with a history of gastric sleeve done two years back who presented to the emergency department with complaints of worsening abdominal pain for 3 weeks. Computed tomography abdomen showed post-surgical gastric sleeve changes with new ill-defined fluid containing cavities around the staple line, perigastric thickening, and gastrosplenic ligament edema. This was confirmed by an esophagram that also showed fluid-filled density (3.3cm) along the posterior aspect of the stomach connecting to the proximal stomach. Endoscopy revealed a disrupted sleeve gastrectomy staple line at two different areas with a larger proximal and smaller distal abscess cavity. Pus was exuding from the cavities, and both areas were irrigated. We intentionally connected the two cavities with guide wire-assisted blunt dissection. A fully covered 10x10 Viabil stent was used as an out-in-stent to bypass the abscess cavities under fluoroscopic guidance. The stent exited the sleeve, bypassed the proximal and the distal cavities, and reentered the sleeve lumen from the distal abscess cavity. The stent was secured with sutures. The patient has remained symptom-free for 3 months and the stent was removed. Fluoroscopic imaging showed no contrast extending the gastric lumen and previous fistula opening had closed.
Discussion: We show a novel management approach to manage abscess cavities at disrupted staple line using extraluminal out-in-stent.
Figure: A-Preadmission CT scan showing ill-defined fluid collection next to sleeve.
B- esophagram confirming the fluid filled density along the posterior aspect of the upper stomach.
C- esophagram showing the stent in-situ as an in-out stent (yellow arrow)
D- esophagram showing absence of leak.
B- esophagram confirming the fluid filled density along the posterior aspect of the upper stomach.
C- esophagram showing the stent in-situ as an in-out stent (yellow arrow)
D- esophagram showing absence of leak.
Disclosures:
Mayank Goyal indicated no relevant financial relationships.
Ashwariya Ohri indicated no relevant financial relationships.
Anmol Bains indicated no relevant financial relationships.
Yadwinder Singh indicated no relevant financial relationships.
Laurens Janssens indicated no relevant financial relationships.
Navtej Buttar indicated no relevant financial relationships.
Mayank Goyal, MBBS, Ashwariya Ohri, MBBS, Anmol Bains, MBBS, Yadwinder Singh, MBBS, Laurens Janssens, MD, Navtej Buttar, MD. P3892 - EBACS (Endoscopic Bypass of Abscess With Covered Stent), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
