Tuesday Poster Session
Category: Endoscopy Video Forum
P3894 - Management of Gastrojejunal Obstruction Using Coupled Fully Covered Self Expanding Metal Stents
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AK
Andrew Kleehammer, DO
University of Florida College of Medicine
Gainesville, FL
Presenting Author(s)
Andrew Kleehammer, DO1, Katarina Pittman, MD1, Jennifer Fieber, MD1, Ibrahim Nassour, MD1, Aleksey Novikov, MD2
1University of Florida College of Medicine, Gainesville, FL; 2University of Florida, Gainesville, FL
Introduction: Fully covered self-expanding metal stents (FCSEMS) are frequently used in the therapeutic endoscopic management of esophageal and biliary strictures. Stent migration is a known complication of FCSEMS. This case highlights an off-label use of esophageal FCSEMS and a novel approach to prevent stent migration.
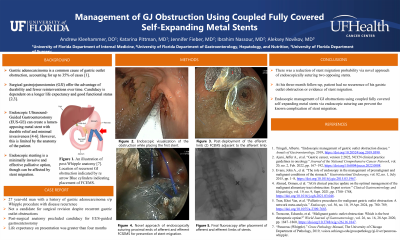
Case Description/Methods: This is a case of a 26-year-old man with history of gastric adenocarcinoma status post Whipple procedure and adjuvant chemotherapy with a post-operative course complicated by GJ anastomotic stricture and recurrent gastric outlet obstruction. The patient presented with nausea and vomiting with poor oral intake tolerance. The patient was deemed to not be a candidate for further surgical revision. Due to his post-surgical anatomy, the patient was not a candidate for endoscopic ultrasound-guided gastroenterostomy. However, he was judged to have a life expectancy of greater than 4 months. Esophagogastroduodenoscopy (EGD) was performed with evidence of stricture of the gastrojejunostomy (GJ) anastomosis with stricture leading to the afferent jejunal loop and the efferent jejunal loop. Both strictures were traversed with a guidewire and then an esophageal FCSEMS with stent deployment under endoscopic and fluoroscopic guidance. To prevent stent migration an endoscopic suturing device was used to anchor each stent to the gastric wall and two 2-0 polypropylene sutures were placed in a running fashion to fix each stent to the mucosa. The decision was made to use the endoscopic suturing device to suture the 2 stents to each other to minimize the risk of stent migration and a single suture was placed to interlock the 2 stents. The patient tolerated the procedure well. He could tolerate oral intake post-procedure and his symptoms of nausea and vomiting resolved. Upon discharge he continued following with his primary oncology team and had no evidence of gastric outlet obstruction or residual symptoms at 3 months post-procedure follow-up.
Discussion: In this case, we used endoscopic suturing to interlock 2 esophageal fully covered self-expanding metal stents placed across the patient’s GJ anastomotic stricture as an off-label therapy for recurrent gastric outlet obstruction in Whipple anatomy. This represents a novel approach to endoscopic therapy in those patients who are not candidates for other interventions and presents a solution to the known complication of FCEMS migration.
Disclosures:
Andrew Kleehammer, DO1, Katarina Pittman, MD1, Jennifer Fieber, MD1, Ibrahim Nassour, MD1, Aleksey Novikov, MD2. P3894 - Management of Gastrojejunal Obstruction Using Coupled Fully Covered Self Expanding Metal Stents, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Florida College of Medicine, Gainesville, FL; 2University of Florida, Gainesville, FL
Introduction: Fully covered self-expanding metal stents (FCSEMS) are frequently used in the therapeutic endoscopic management of esophageal and biliary strictures. Stent migration is a known complication of FCSEMS. This case highlights an off-label use of esophageal FCSEMS and a novel approach to prevent stent migration.
Case Description/Methods: This is a case of a 26-year-old man with history of gastric adenocarcinoma status post Whipple procedure and adjuvant chemotherapy with a post-operative course complicated by GJ anastomotic stricture and recurrent gastric outlet obstruction. The patient presented with nausea and vomiting with poor oral intake tolerance. The patient was deemed to not be a candidate for further surgical revision. Due to his post-surgical anatomy, the patient was not a candidate for endoscopic ultrasound-guided gastroenterostomy. However, he was judged to have a life expectancy of greater than 4 months. Esophagogastroduodenoscopy (EGD) was performed with evidence of stricture of the gastrojejunostomy (GJ) anastomosis with stricture leading to the afferent jejunal loop and the efferent jejunal loop. Both strictures were traversed with a guidewire and then an esophageal FCSEMS with stent deployment under endoscopic and fluoroscopic guidance. To prevent stent migration an endoscopic suturing device was used to anchor each stent to the gastric wall and two 2-0 polypropylene sutures were placed in a running fashion to fix each stent to the mucosa. The decision was made to use the endoscopic suturing device to suture the 2 stents to each other to minimize the risk of stent migration and a single suture was placed to interlock the 2 stents. The patient tolerated the procedure well. He could tolerate oral intake post-procedure and his symptoms of nausea and vomiting resolved. Upon discharge he continued following with his primary oncology team and had no evidence of gastric outlet obstruction or residual symptoms at 3 months post-procedure follow-up.
Discussion: In this case, we used endoscopic suturing to interlock 2 esophageal fully covered self-expanding metal stents placed across the patient’s GJ anastomotic stricture as an off-label therapy for recurrent gastric outlet obstruction in Whipple anatomy. This represents a novel approach to endoscopic therapy in those patients who are not candidates for other interventions and presents a solution to the known complication of FCEMS migration.
Disclosures:
Andrew Kleehammer indicated no relevant financial relationships.
Katarina Pittman indicated no relevant financial relationships.
Jennifer Fieber indicated no relevant financial relationships.
Ibrahim Nassour indicated no relevant financial relationships.
Aleksey Novikov indicated no relevant financial relationships.
Andrew Kleehammer, DO1, Katarina Pittman, MD1, Jennifer Fieber, MD1, Ibrahim Nassour, MD1, Aleksey Novikov, MD2. P3894 - Management of Gastrojejunal Obstruction Using Coupled Fully Covered Self Expanding Metal Stents, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
