Tuesday Poster Session
Category: Esophagus
P3895 - Esophageal Motility in Patients With Primary Hyperparathyroidism
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- HS
Hasan Saleh, MD, MBA
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Hasan Saleh, MD, MBA, Maoyin Pang, MD, PhD
Mayo Clinic, Jacksonville, FL
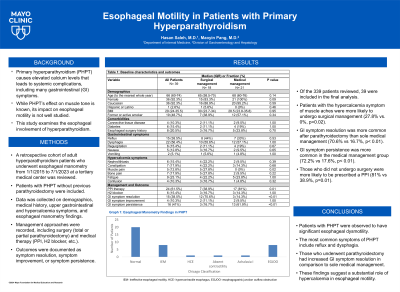
Introduction: Primary hyperparathyroidism (PHPT) causes elevated calcium levels that leads to systemic complications, including the gastrointestinal symptoms. While PHPT’s effect on muscle tone is known, its impact on esophageal motility is not well studied. This study examines the esophageal involvement of hyperparathyroidism.
Methods: A retrospective cohort of adult hyperparathyroidism patients who underwent esophageal manometry from 1/1/2015 to 7/1/2023 at a tertiary medical center was reviewed. Patients with PHPT without previous parathyroidectomy were included. Data was collected on demographics, medical history, upper gastrointestinal and hypercalcemia symptoms, and esophageal manometry. Management approaches were recorded, including surgery (total or partial parathyroidectomy) and medical therapy (PPI, H2 blocker, etc.). Outcomes were documented as symptom resolution, symptom improvement, or symptom persistence.
Results: Of the 339 patients reviewed, 39 were included in the final analysis. Esophageal manometry findings were normal motility (n=20), ineffective esophageal motility (n=8), esophagogastric junction outflow obstruction (n=8), hypercontractile esophagus (n=1), absent contractility (n=1), and achalasia I (n=1). Median serum calcium levels were 10.5 mg/dL (8.8-10.2). The most common gastrointestinal symptoms were reflux (38%) and dysphagia (56%).
Eighteen patients underwent parathyroidectomy whereas 21 had sole medical management. There were no differences in presenting gastrointestinal symptoms between the surgical and medical groups. Patients with the hypercalcemia symptom of muscle aches were more likely to undergo surgical management (27.8% vs. 0%, p=0.02).
Symptom resolution was more common after parathyroidectomy than sole medical management (70.6% vs 16.7%, p< 0.01). Symptom persistence was more common in the medical management group (72.2% vs 17.6%, p< 0.01). Those who did not undergo surgery were more likely to be prescribed a PPI (81% vs 38.9%, p=0.01).
Discussion: Patients with PHPT were observed to have significant esophageal dysmotility with symptoms of reflux and dysphagia. Those who underwent parathyroidectomy had increased symptom resolution. These findings suggest a substantial role of hypercalcemia in esophageal motility.
Disclosures:
Hasan Saleh, MD, MBA, Maoyin Pang, MD, PhD. P3895 - Esophageal Motility in Patients With Primary Hyperparathyroidism, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Jacksonville, FL
Introduction: Primary hyperparathyroidism (PHPT) causes elevated calcium levels that leads to systemic complications, including the gastrointestinal symptoms. While PHPT’s effect on muscle tone is known, its impact on esophageal motility is not well studied. This study examines the esophageal involvement of hyperparathyroidism.
Methods: A retrospective cohort of adult hyperparathyroidism patients who underwent esophageal manometry from 1/1/2015 to 7/1/2023 at a tertiary medical center was reviewed. Patients with PHPT without previous parathyroidectomy were included. Data was collected on demographics, medical history, upper gastrointestinal and hypercalcemia symptoms, and esophageal manometry. Management approaches were recorded, including surgery (total or partial parathyroidectomy) and medical therapy (PPI, H2 blocker, etc.). Outcomes were documented as symptom resolution, symptom improvement, or symptom persistence.
Results: Of the 339 patients reviewed, 39 were included in the final analysis. Esophageal manometry findings were normal motility (n=20), ineffective esophageal motility (n=8), esophagogastric junction outflow obstruction (n=8), hypercontractile esophagus (n=1), absent contractility (n=1), and achalasia I (n=1). Median serum calcium levels were 10.5 mg/dL (8.8-10.2). The most common gastrointestinal symptoms were reflux (38%) and dysphagia (56%).
Eighteen patients underwent parathyroidectomy whereas 21 had sole medical management. There were no differences in presenting gastrointestinal symptoms between the surgical and medical groups. Patients with the hypercalcemia symptom of muscle aches were more likely to undergo surgical management (27.8% vs. 0%, p=0.02).
Symptom resolution was more common after parathyroidectomy than sole medical management (70.6% vs 16.7%, p< 0.01). Symptom persistence was more common in the medical management group (72.2% vs 17.6%, p< 0.01). Those who did not undergo surgery were more likely to be prescribed a PPI (81% vs 38.9%, p=0.01).
Discussion: Patients with PHPT were observed to have significant esophageal dysmotility with symptoms of reflux and dysphagia. Those who underwent parathyroidectomy had increased symptom resolution. These findings suggest a substantial role of hypercalcemia in esophageal motility.
Disclosures:
Hasan Saleh indicated no relevant financial relationships.
Maoyin Pang indicated no relevant financial relationships.
Hasan Saleh, MD, MBA, Maoyin Pang, MD, PhD. P3895 - Esophageal Motility in Patients With Primary Hyperparathyroidism, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
