Tuesday Poster Session
Category: Esophagus
P3896 - Efficacy and Safety of Radiofrequency Ablation in Management of Patients With Low-Grade Dysplasia in Barrett's Esophagus: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SK
Shahryar Khan, MD
University of Kansas
Overland Park, KS
Presenting Author(s)
Shahryar Khan, MD1, Ahmad Khan, MBBS2, Hamza Asif, MD3, Fatma Hussain, MBBS4, Mashal Alam Khan, MBBS5, Aamer Ahmad, MBBS6
1University of Kansas, Overland Park, KS; 2Khyber Teaching Hospital, Nowshera, North-West Frontier, Pakistan; 3Khyber Teaching Hospital, Peshawar, North-West Frontier, Pakistan; 4Khyber Medical College Peshawar affiliated with Khyber Medical University, Swat, North-West Frontier, Pakistan; 5Khyber Medical University, Overland Park, KS; 6Khyber Medical University, Peshawar, North-West Frontier, Pakistan
Introduction: Low grade dysplasia in Barrett's Esophagus (BE-LG) is associated with an increasing risk of developing high grade dysplasia (HGD) and esophageal carcinoma (EC). Patients undergo endoscopic surveillance or treatment, depending on the presence and grade of dysplasia. However, the management of BE-LG is still debatable because it can be over diagnosed, and the risk of progression to HGD and EC is uncertain. Radiofrequency ablation (RFA) can eradicate dysplasia and intestinal metaplasia in patients with dysplastic Barrett’s esophagus (BE) and reduce rates of esophageal adenocarcinoma. We aimed to perform a systematic review and meta-analysis of studies that evaluated the efficacy of RFA for the treatment of BE-LG and comparison with endoscopic surveillance (ES).
Methods: We systematically searched PubMed and Embase to identify relevant studies published from inception through June 2024. The outcomes of interest were Complete Eradication of Dysplasia (CE-D), Complete Eradication of Intestinal Metaplasia (CE-IM), Adverse Events (AEs), Risk of Progression to HGD, and EC. The random effects model was used to calculate the pooled mean effect (PME) and odds ratio (OR) with the corresponding 95% confidence intervals of our desired outcomes. Heterogeneity was assessed using the I2 Index. Qualities of studies were assessed using the ROBINS-1 tool. Data analysis was performed using Revman and MedCalc softwares.
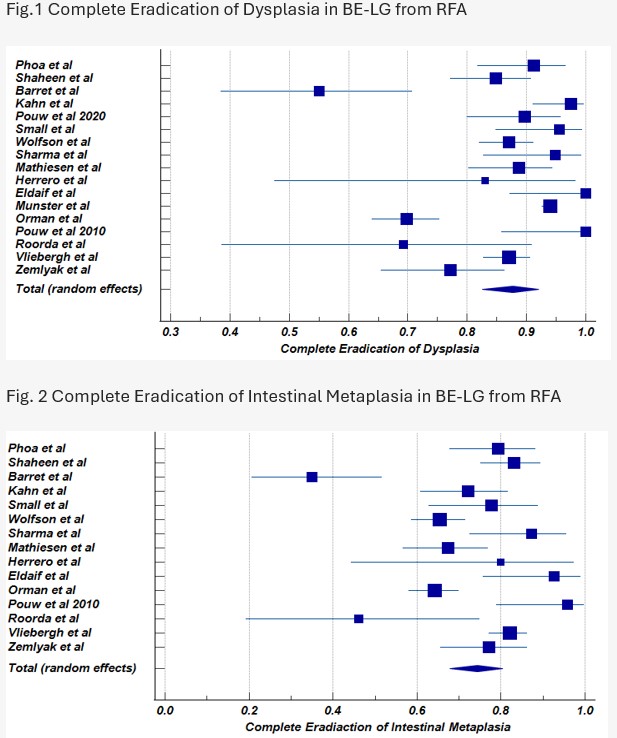
Results: In our meta-analysis, 14 non-RCTs and 3 RCTs were included with a total population of 3327. Participants comprise an Average age of 65.2, Female 19.50%, Average BMI of 28 and mean follow up duration was 28 months. CE-D was achieved with PME 87.70%, 95% CI 82.57-92.04, I2 = 90.69%, P < 0.05 (Fig.1), CE-D with PME 74.37%, 95% CI 67.8-80.4, I2 = 84.4%, P < 0.05 (Fig.2) in BE-LG from RFA. Most common reported AEs with RFA was esophageal structures (11.5%). Comparing with ES, RFA is associated with higher CE-D (OR 10.15, 95% CI 1.55 to 66.5, I2 = 87%, P = 0.006), lower risk of progression to HGD (OR 0.21, 95% CI 0.09 to 0.51, I2 = 42%, P < 0.05), and lower risk of progression to EC (OR 0.32, 95% CI 0.11 to 0.97, I2 = 16%, P 0.04).
Discussion: Our study showed that RFA is effective for eradication of BE-LG, significantly lowering rates of progression to HGD and EC in comparison with ES. However, Larger multicenter and longer follow-up studies with systematic approach are warranted to validate these findings.
Disclosures:
Shahryar Khan, MD1, Ahmad Khan, MBBS2, Hamza Asif, MD3, Fatma Hussain, MBBS4, Mashal Alam Khan, MBBS5, Aamer Ahmad, MBBS6. P3896 - Efficacy and Safety of Radiofrequency Ablation in Management of Patients With Low-Grade Dysplasia in Barrett's Esophagus: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kansas, Overland Park, KS; 2Khyber Teaching Hospital, Nowshera, North-West Frontier, Pakistan; 3Khyber Teaching Hospital, Peshawar, North-West Frontier, Pakistan; 4Khyber Medical College Peshawar affiliated with Khyber Medical University, Swat, North-West Frontier, Pakistan; 5Khyber Medical University, Overland Park, KS; 6Khyber Medical University, Peshawar, North-West Frontier, Pakistan
Introduction: Low grade dysplasia in Barrett's Esophagus (BE-LG) is associated with an increasing risk of developing high grade dysplasia (HGD) and esophageal carcinoma (EC). Patients undergo endoscopic surveillance or treatment, depending on the presence and grade of dysplasia. However, the management of BE-LG is still debatable because it can be over diagnosed, and the risk of progression to HGD and EC is uncertain. Radiofrequency ablation (RFA) can eradicate dysplasia and intestinal metaplasia in patients with dysplastic Barrett’s esophagus (BE) and reduce rates of esophageal adenocarcinoma. We aimed to perform a systematic review and meta-analysis of studies that evaluated the efficacy of RFA for the treatment of BE-LG and comparison with endoscopic surveillance (ES).
Methods: We systematically searched PubMed and Embase to identify relevant studies published from inception through June 2024. The outcomes of interest were Complete Eradication of Dysplasia (CE-D), Complete Eradication of Intestinal Metaplasia (CE-IM), Adverse Events (AEs), Risk of Progression to HGD, and EC. The random effects model was used to calculate the pooled mean effect (PME) and odds ratio (OR) with the corresponding 95% confidence intervals of our desired outcomes. Heterogeneity was assessed using the I2 Index. Qualities of studies were assessed using the ROBINS-1 tool. Data analysis was performed using Revman and MedCalc softwares.
Results: In our meta-analysis, 14 non-RCTs and 3 RCTs were included with a total population of 3327. Participants comprise an Average age of 65.2, Female 19.50%, Average BMI of 28 and mean follow up duration was 28 months. CE-D was achieved with PME 87.70%, 95% CI 82.57-92.04, I2 = 90.69%, P < 0.05 (Fig.1), CE-D with PME 74.37%, 95% CI 67.8-80.4, I2 = 84.4%, P < 0.05 (Fig.2) in BE-LG from RFA. Most common reported AEs with RFA was esophageal structures (11.5%). Comparing with ES, RFA is associated with higher CE-D (OR 10.15, 95% CI 1.55 to 66.5, I2 = 87%, P = 0.006), lower risk of progression to HGD (OR 0.21, 95% CI 0.09 to 0.51, I2 = 42%, P < 0.05), and lower risk of progression to EC (OR 0.32, 95% CI 0.11 to 0.97, I2 = 16%, P 0.04).
Discussion: Our study showed that RFA is effective for eradication of BE-LG, significantly lowering rates of progression to HGD and EC in comparison with ES. However, Larger multicenter and longer follow-up studies with systematic approach are warranted to validate these findings.
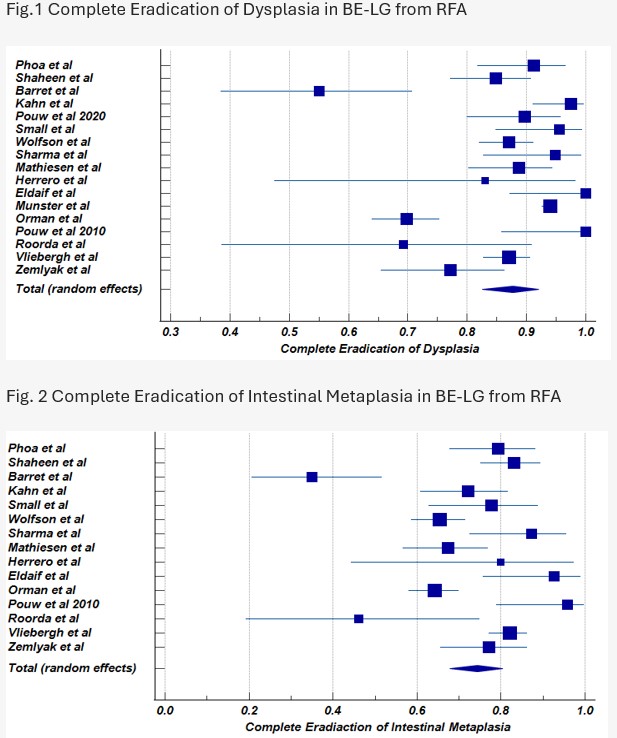
Figure: Forrest Plots. Fig.1 and Fig.2
Disclosures:
Shahryar Khan indicated no relevant financial relationships.
Ahmad Khan indicated no relevant financial relationships.
Hamza Asif indicated no relevant financial relationships.
Fatma Hussain indicated no relevant financial relationships.
Mashal Alam Khan indicated no relevant financial relationships.
Aamer Ahmad indicated no relevant financial relationships.
Shahryar Khan, MD1, Ahmad Khan, MBBS2, Hamza Asif, MD3, Fatma Hussain, MBBS4, Mashal Alam Khan, MBBS5, Aamer Ahmad, MBBS6. P3896 - Efficacy and Safety of Radiofrequency Ablation in Management of Patients With Low-Grade Dysplasia in Barrett's Esophagus: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
