Tuesday Poster Session
Category: Esophagus
P3898 - A Comparison of the 3 Subtypes of Achalasia Using High Resolution Manometry, Timed Barium Esophagram, and EndoFLIP
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AJ
Anuj Jailwala, BSc
Wake Forest University School of Medicine
Winston-Salem, NC
Presenting Author(s)
Anuj Jailwala, BSc, Anthony Wachnik, BSc, Chiagoziem Ogbonna, MD, Makell Brown, BSPH, Steven Clayton, MD
Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Achalasia is an esophageal motility disorder characterized by lack of peristalsis and impaired relaxation of the lower esophageal sphincter during swallowing. High-resolution esophageal manometry (HRM) is the gold standard diagnostic test and uses the Chicago classification system to sub-classify Achalasia into Types I (absent peristalsis), II (panesophageal pressurization), and III (premature contractions). Timed barium esophagram (TBE) and endoscopic functional luminal imaging probe (EndoFLIP) are complimentary tools for aiding in the diagnosis of Achalasia. The aim of our study was to examine differences in HRM, TBE, and EndoFLIP findings between the three Achalasia subtypes.
Methods: Our study includes all patients age >18 who have had HRM studies done at our facility in the last 5 years. A review of the electronic medical records identified patients with the manometric diagnosis of Achalasia who had TBE/EndoFLIP performed. Where appropriate, Fisher’s exact test and Pearson’s chi-squared test were used for categorical covariates whereas the Wilcoxon and Kruskal-Wallis rank sum tests were used for continuous covariates of interest across the groups.
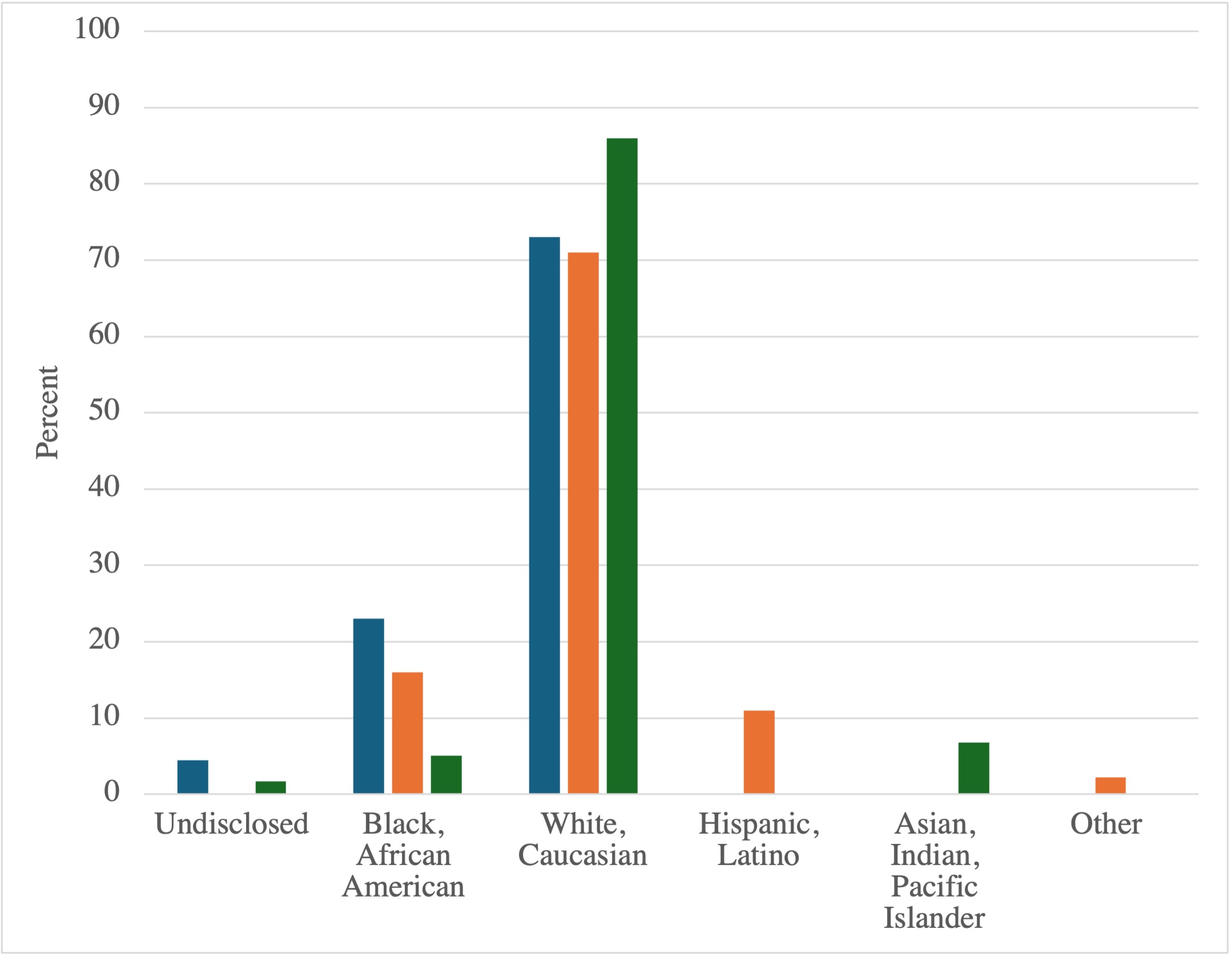
Results: Of the 1506 patients who underwent HRM since 2018, 126 (8.37%) met HRM criteria for Achalasia types I-III. As shown in Figure 1, there was a significant difference in patients that met criteria on HRM based on race, with White, Caucasian being the most represented across all three groups (p=0.003). 73 (58%) of the cases were followed up with supportive investigations. As shown in Table 1, the HRM LES basal pressure (p=0.038), residual pressure (p< 0.001), and DCI (p< 0.001) were significantly higher in types II and III Achalasia. There was no significant difference in the height of the TBE column at 1 min (p=0.88) or tablet passage (p=0.92) between the three groups. On EndoFLIP analysis, there was a significantly higher balloon pressure at a 60 mL fill volume for patients with types II and III Achalasia (< 0.001) but no difference in distensibility index (p=0.50) or contractile response pattern between the three subtypes (p=0.092).
Discussion: Our major findings suggest that manometrically type III Achalasia tended to have higher LES basal and residual pressures compared to type I and type II Achalasia on HRM. There was no difference in the height of the barium column between the three subtypes on TBE. Type III Achalasia tended to have a higher balloon pressure at a 60 mL fill volume compared to types I and II Achalasia.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anuj Jailwala, BSc, Anthony Wachnik, BSc, Chiagoziem Ogbonna, MD, Makell Brown, BSPH, Steven Clayton, MD. P3898 - A Comparison of the 3 Subtypes of Achalasia Using High Resolution Manometry, Timed Barium Esophagram, and EndoFLIP, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Achalasia is an esophageal motility disorder characterized by lack of peristalsis and impaired relaxation of the lower esophageal sphincter during swallowing. High-resolution esophageal manometry (HRM) is the gold standard diagnostic test and uses the Chicago classification system to sub-classify Achalasia into Types I (absent peristalsis), II (panesophageal pressurization), and III (premature contractions). Timed barium esophagram (TBE) and endoscopic functional luminal imaging probe (EndoFLIP) are complimentary tools for aiding in the diagnosis of Achalasia. The aim of our study was to examine differences in HRM, TBE, and EndoFLIP findings between the three Achalasia subtypes.
Methods: Our study includes all patients age >18 who have had HRM studies done at our facility in the last 5 years. A review of the electronic medical records identified patients with the manometric diagnosis of Achalasia who had TBE/EndoFLIP performed. Where appropriate, Fisher’s exact test and Pearson’s chi-squared test were used for categorical covariates whereas the Wilcoxon and Kruskal-Wallis rank sum tests were used for continuous covariates of interest across the groups.
Results: Of the 1506 patients who underwent HRM since 2018, 126 (8.37%) met HRM criteria for Achalasia types I-III. As shown in Figure 1, there was a significant difference in patients that met criteria on HRM based on race, with White, Caucasian being the most represented across all three groups (p=0.003). 73 (58%) of the cases were followed up with supportive investigations. As shown in Table 1, the HRM LES basal pressure (p=0.038), residual pressure (p< 0.001), and DCI (p< 0.001) were significantly higher in types II and III Achalasia. There was no significant difference in the height of the TBE column at 1 min (p=0.88) or tablet passage (p=0.92) between the three groups. On EndoFLIP analysis, there was a significantly higher balloon pressure at a 60 mL fill volume for patients with types II and III Achalasia (< 0.001) but no difference in distensibility index (p=0.50) or contractile response pattern between the three subtypes (p=0.092).
Discussion: Our major findings suggest that manometrically type III Achalasia tended to have higher LES basal and residual pressures compared to type I and type II Achalasia on HRM. There was no difference in the height of the barium column between the three subtypes on TBE. Type III Achalasia tended to have a higher balloon pressure at a 60 mL fill volume compared to types I and II Achalasia.
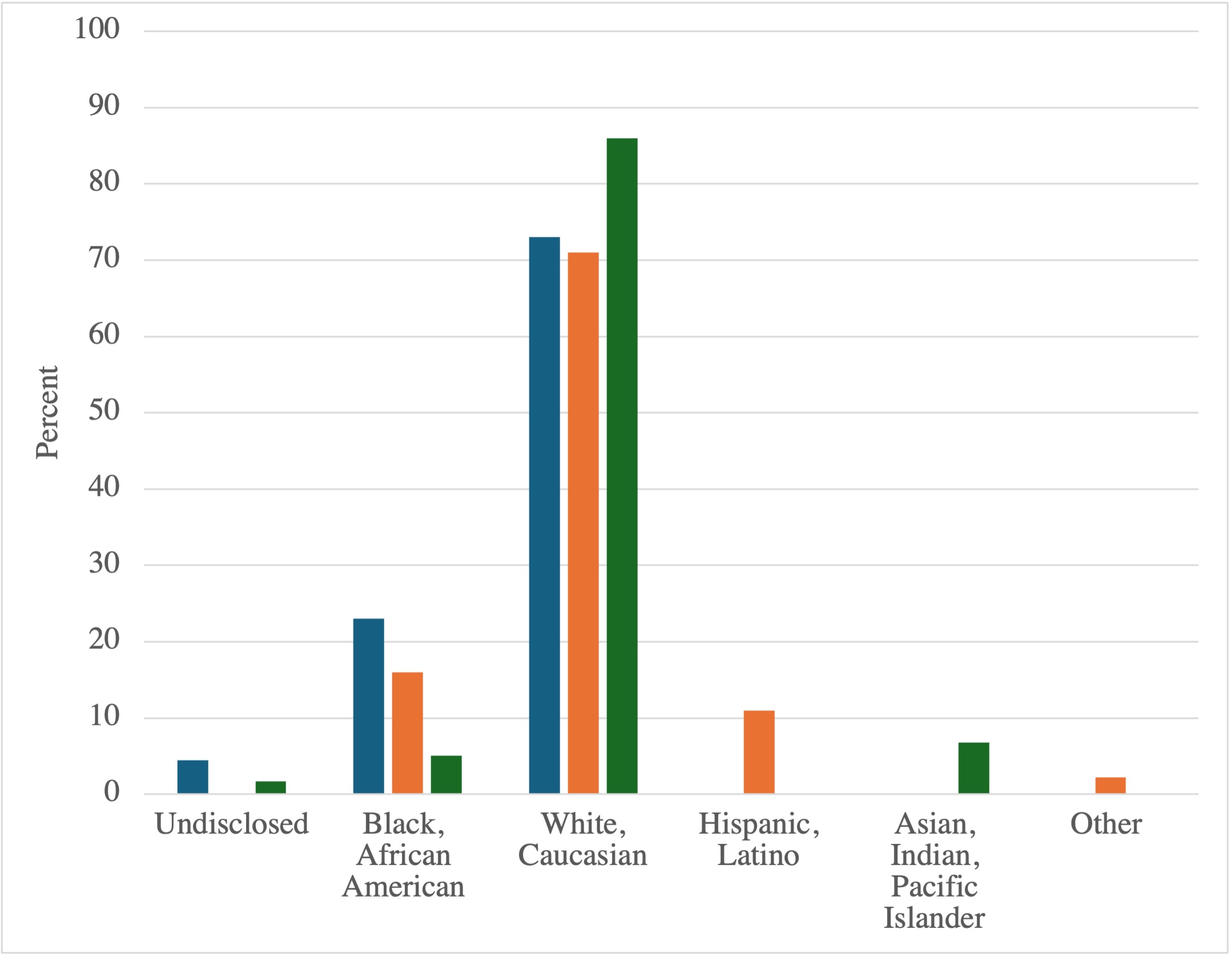
Figure: Figure 1- Breakdown by race of patients meeting HRM criteria for Achalasia I, II, or III (Blue= Achalasia I, Orange= Achalasia II, Green= Achalasia III)
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anuj Jailwala indicated no relevant financial relationships.
Anthony Wachnik indicated no relevant financial relationships.
Chiagoziem Ogbonna indicated no relevant financial relationships.
Makell Brown indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
Anuj Jailwala, BSc, Anthony Wachnik, BSc, Chiagoziem Ogbonna, MD, Makell Brown, BSPH, Steven Clayton, MD. P3898 - A Comparison of the 3 Subtypes of Achalasia Using High Resolution Manometry, Timed Barium Esophagram, and EndoFLIP, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
