Tuesday Poster Session
Category: Colorectal Cancer Prevention
P3824 - Direct Genetic Screening Approach in Hereditary Nonpolyposis Colorectal Cancer: A Health Economics Analysis in High-risk Colorectal Cancer Population; Perspective from Middle-Income Country
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Pongtawat Lertwilaiwittaya, MD
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Pongtawat Lertwilaiwittaya, MD1, Natthakan Chitpim, PharmD2, Pattara Leelahavarong, PhD2, Vitcha Poonyakanok, MD2, Suchapa Arayakarnkul, MD3, Manop Pithukpakorn, MD2, Varalak Srinonprasert, MD2
1University of Alabama at Birmingham, Birmingham, AL; 2Siriraj Hospital, Mahidol University, Bangkoknoi, Krung Thep, Thailand; 3University of Minnesota, Minneapolis, MN
Introduction: The prevalence of Hereditary Nonpolyposis Colorectal Cancer syndrome (Lynch syndrome, LS) was estimated to be 3-5% of all colorectal cancer. Molecular diagnosis of LS helps guide cancer surveillance, immune checkpoint inhibitor eligibility, and familial cascade testing. Universal tumor mismatch repair protein immunohistochemistry was proposed to increase LS detection; however, this has been a logistical challenge with less than 50% rate of screening. Prior efforts at direct genetics screening approach have never shown cost-effectiveness acceptability. Our team aims to pilot health economics analysis of direct LS genetic screening in high-risk colorectal cancer patients (per NCCN guidelines version 1.2020) in a middle-income country setting, Thailand.
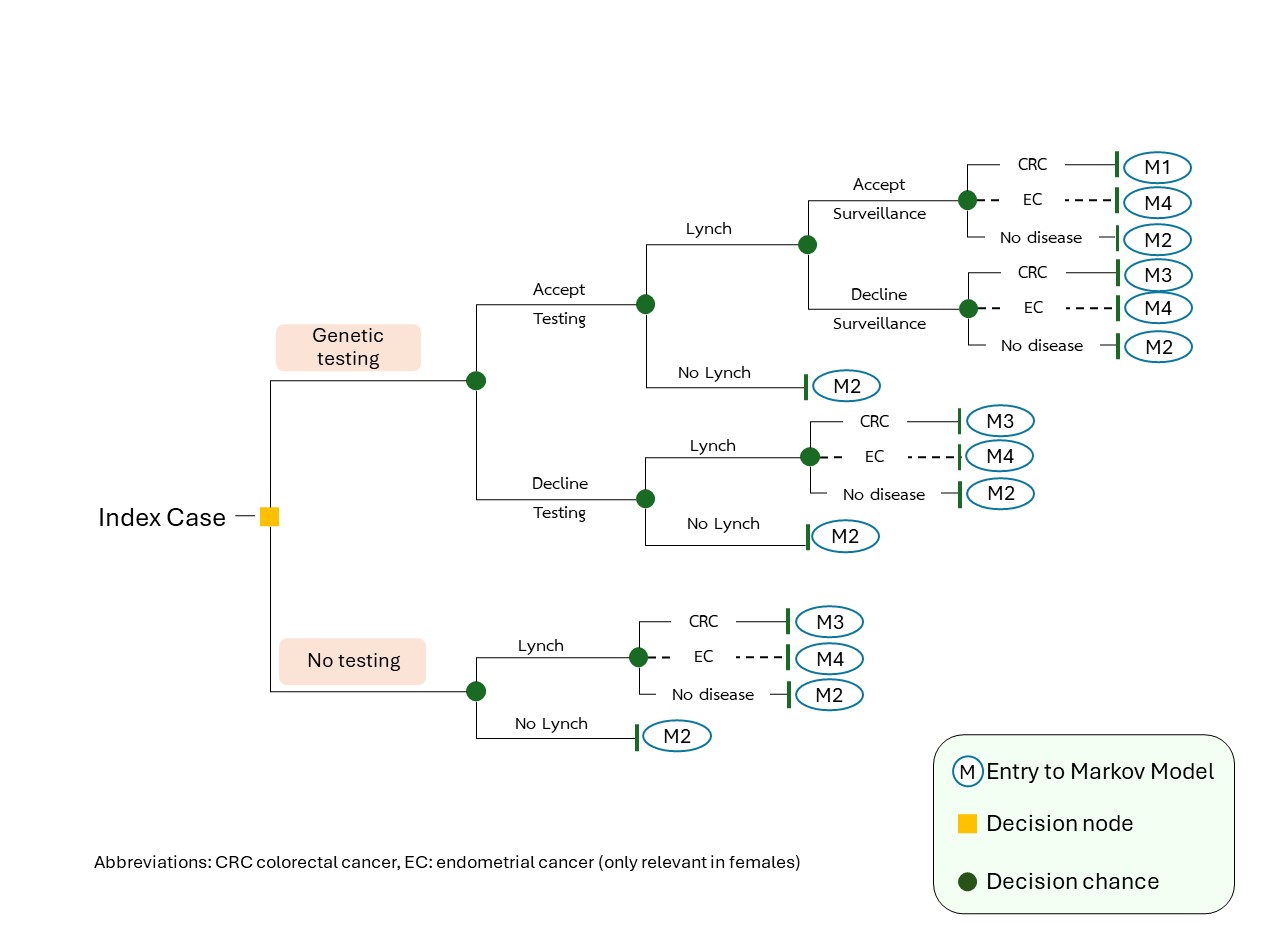
Methods: Decision tree (Figure 1) and Markov model were utilized to assess health outcomes and costs using a lifetime horizon from a societal perspective. The model took into consideration the colorectal and endometrial cancer risk differences between genders. Local data were prioritized at each transitional probability. 56 endometrial cancer patients were interviewed to address missing relevant costs and quality of life using the EQ-5D-5L questionnaire.
Results: The genetic screening strategy was estimated to pose a $114 incremental lifetime cost, 2 life years (LY), and 2 quality-adjusted life years (QALY) gained in comparison to the no-testing strategy. The incremental cost-utility ratio of genetic screening in the high-risk patients was $55.96/LY and $55.35/QALY. In family members, the genetic screening strategy led to -$306 incremental lifetime cost, 2.3 LY, and 2.3 QALY gained. It was cost-saving to do familial cascade testing (Table 1). In subgroup analysis, genetics testing in high-risk female populations was cost-saving (-$417.10/LY and -$402.84/QALY).
Discussion: Our study highlighted a highly cost-effective and cost-utility perspective of germline LS screening in high-risk cancer patients (including diagnosis of colorectal cancer before 50 years of age, synchronous and metachronous cancer) especially in female patients. Expanding the program to family members was cost-saving. We strongly encourage the endorsement of LS genetics testing in high-risk cancer patients and their family members under national healthcare benefits. Other resource-limited countries should consider the direct genetic testing approach as an additional option.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Pongtawat Lertwilaiwittaya, MD1, Natthakan Chitpim, PharmD2, Pattara Leelahavarong, PhD2, Vitcha Poonyakanok, MD2, Suchapa Arayakarnkul, MD3, Manop Pithukpakorn, MD2, Varalak Srinonprasert, MD2. P3824 - Direct Genetic Screening Approach in Hereditary Nonpolyposis Colorectal Cancer: A Health Economics Analysis in High-risk Colorectal Cancer Population; Perspective from Middle-Income Country, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham, Birmingham, AL; 2Siriraj Hospital, Mahidol University, Bangkoknoi, Krung Thep, Thailand; 3University of Minnesota, Minneapolis, MN
Introduction: The prevalence of Hereditary Nonpolyposis Colorectal Cancer syndrome (Lynch syndrome, LS) was estimated to be 3-5% of all colorectal cancer. Molecular diagnosis of LS helps guide cancer surveillance, immune checkpoint inhibitor eligibility, and familial cascade testing. Universal tumor mismatch repair protein immunohistochemistry was proposed to increase LS detection; however, this has been a logistical challenge with less than 50% rate of screening. Prior efforts at direct genetics screening approach have never shown cost-effectiveness acceptability. Our team aims to pilot health economics analysis of direct LS genetic screening in high-risk colorectal cancer patients (per NCCN guidelines version 1.2020) in a middle-income country setting, Thailand.
Methods: Decision tree (Figure 1) and Markov model were utilized to assess health outcomes and costs using a lifetime horizon from a societal perspective. The model took into consideration the colorectal and endometrial cancer risk differences between genders. Local data were prioritized at each transitional probability. 56 endometrial cancer patients were interviewed to address missing relevant costs and quality of life using the EQ-5D-5L questionnaire.
Results: The genetic screening strategy was estimated to pose a $114 incremental lifetime cost, 2 life years (LY), and 2 quality-adjusted life years (QALY) gained in comparison to the no-testing strategy. The incremental cost-utility ratio of genetic screening in the high-risk patients was $55.96/LY and $55.35/QALY. In family members, the genetic screening strategy led to -$306 incremental lifetime cost, 2.3 LY, and 2.3 QALY gained. It was cost-saving to do familial cascade testing (Table 1). In subgroup analysis, genetics testing in high-risk female populations was cost-saving (-$417.10/LY and -$402.84/QALY).
Discussion: Our study highlighted a highly cost-effective and cost-utility perspective of germline LS screening in high-risk cancer patients (including diagnosis of colorectal cancer before 50 years of age, synchronous and metachronous cancer) especially in female patients. Expanding the program to family members was cost-saving. We strongly encourage the endorsement of LS genetics testing in high-risk cancer patients and their family members under national healthcare benefits. Other resource-limited countries should consider the direct genetic testing approach as an additional option.
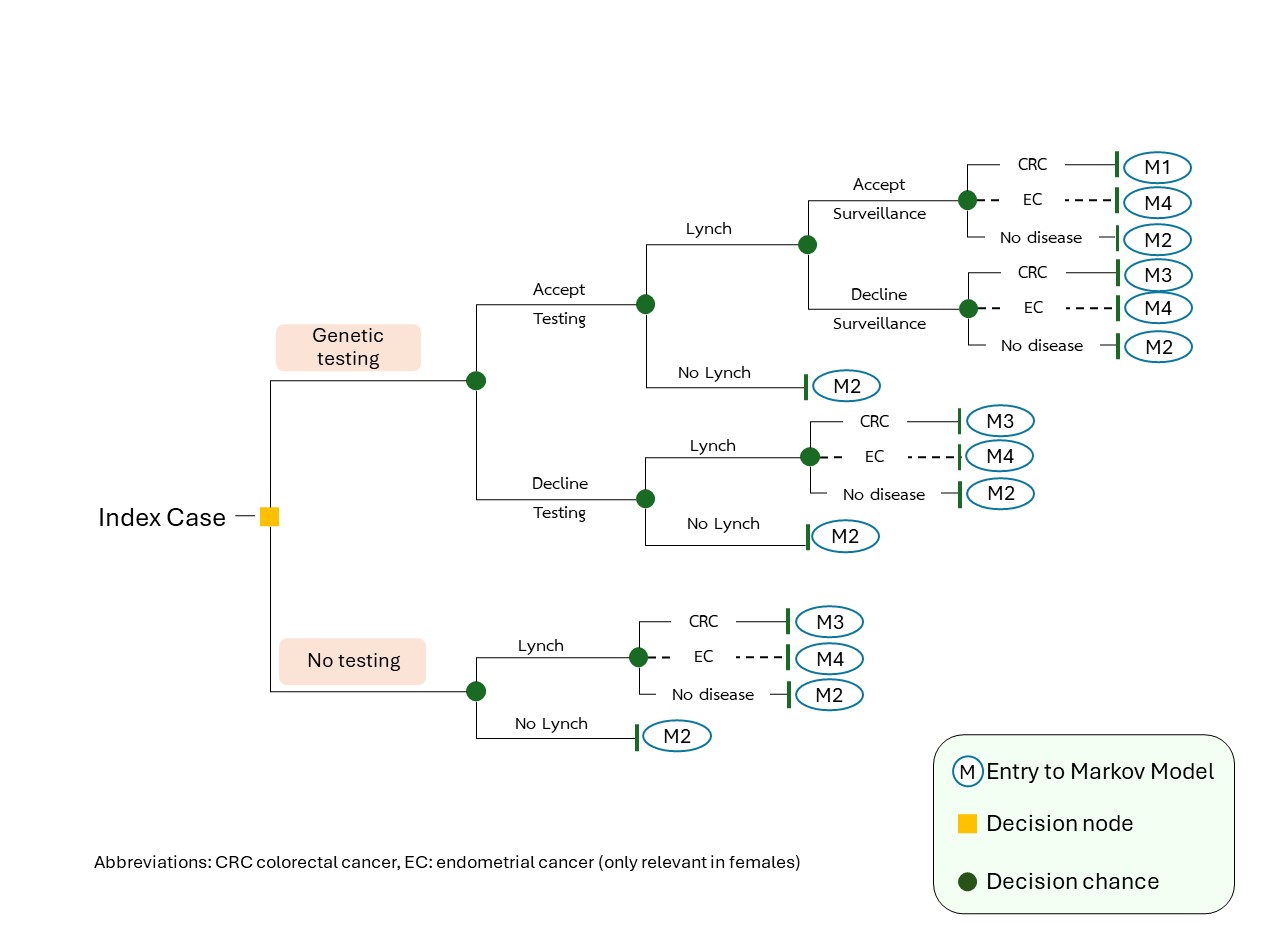
Figure: Figure 1: Hybrid decision tree and Markov model from index case's perspective. Dashed line represents additional-event outcome for endometrial cancer in female population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Pongtawat Lertwilaiwittaya indicated no relevant financial relationships.
Natthakan Chitpim indicated no relevant financial relationships.
Pattara Leelahavarong indicated no relevant financial relationships.
Vitcha Poonyakanok indicated no relevant financial relationships.
Suchapa Arayakarnkul indicated no relevant financial relationships.
Manop Pithukpakorn indicated no relevant financial relationships.
Varalak Srinonprasert indicated no relevant financial relationships.
Pongtawat Lertwilaiwittaya, MD1, Natthakan Chitpim, PharmD2, Pattara Leelahavarong, PhD2, Vitcha Poonyakanok, MD2, Suchapa Arayakarnkul, MD3, Manop Pithukpakorn, MD2, Varalak Srinonprasert, MD2. P3824 - Direct Genetic Screening Approach in Hereditary Nonpolyposis Colorectal Cancer: A Health Economics Analysis in High-risk Colorectal Cancer Population; Perspective from Middle-Income Country, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
