Tuesday Poster Session
Category: Colorectal Cancer Prevention
P3839 - Evaluation of the Impact of Endoscopic Education With Endoscopist-Specific Scorecard Feedback on the Sessile Serrated Lesion Detection Rate (SSLDR)
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Brian E. White, MD
University of Pennsylvania Health System
Philadelphia, PA
Presenting Author(s)
Brian E.. White, MD, Richard M.. Wu, MD, MPH
University of Pennsylvania Health System, Philadelphia, PA
Introduction: The adenoma detection rate (ADR) is a validated quality metric that associates with reduced colorectal cancer risk and has been shown to increase with endoscopist scorecard feedback. The sessile serrated lesion detection rate (SSLDR) is an emerging quality metric sharing a similar inverse association with interval CRC risk, independent of ADR. A new proposed SSLDR benchmark (6%) makes measuring and quality improvement of SSLDR timely and poignant. This study aims to evaluate the impact of endoscopist-specific scorecard feedback with a simultaneous SSL endoscopic educational component on the SSLDR, which is understudied to date.
Methods: This is an interim analysis of a prospective quality improvement project. Baseline SSLDRs and ADRs were obtained over a thirteen-week period using a natural language processing-based tool and validated with manual chart review. Endoscopists were issued scorecards detailing their individual and group quality metrics along with evidence-based practice tips for improving SSLDR at weeks 0 and 13. Baseline and intervention period (weeks 1-23) SSLDR and ADR were compared with chi-squared test. Spearman's rank test was used to assess correlation between quality metrics. Statistical analysis was performed using RStudio 2024.04.1.
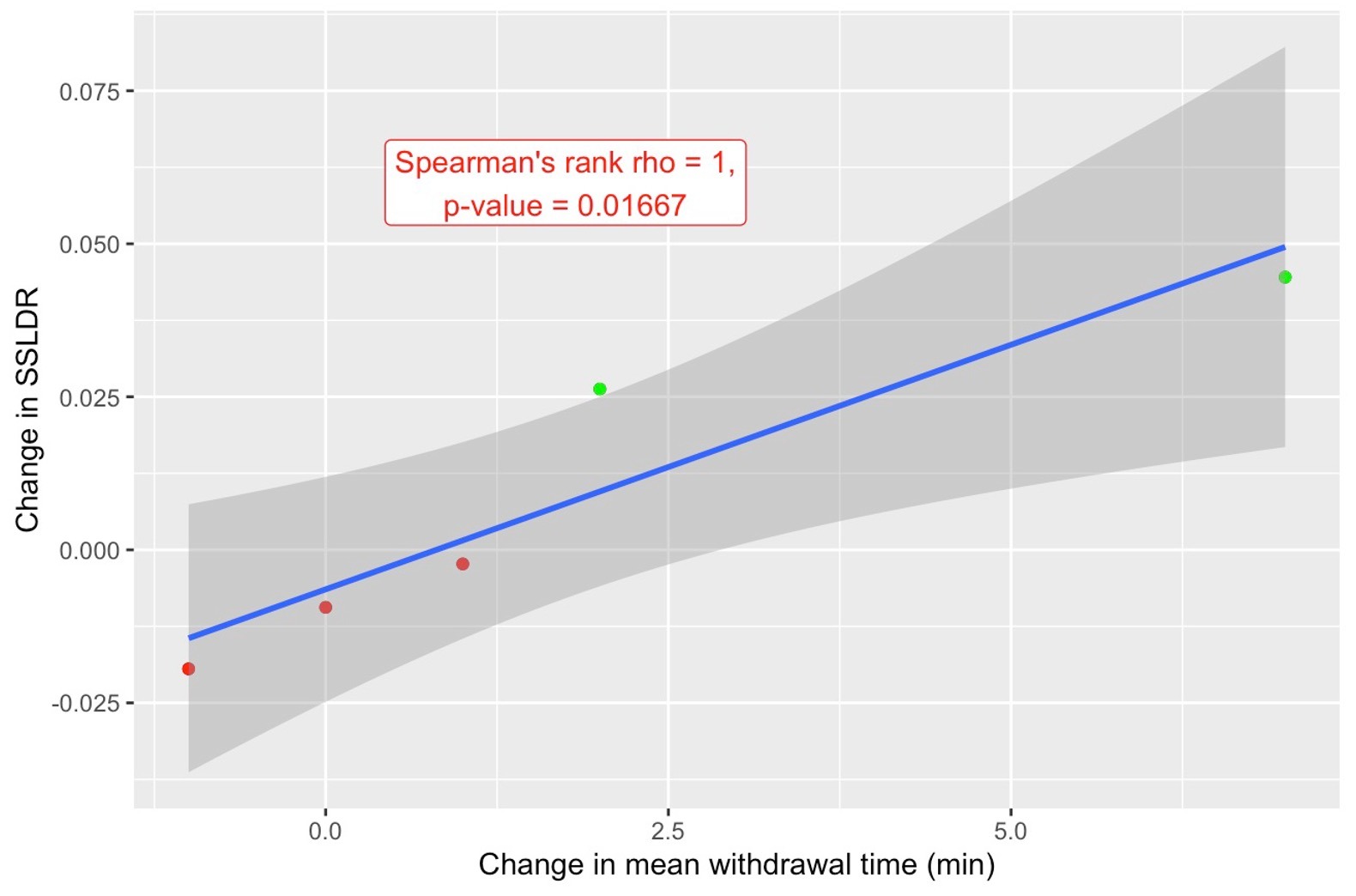
Results: 96 SSLs were detected over 1118 total colonoscopies. Among the group, there were no significant changes in total or screening SSLDR at week 23 compared to baseline (9.5% vs 8.7%, P = 0.65 and 9.4% vs 7.9%, P = 0.69). Two of five endoscopists had non-significant increases in total SSLDR at week 23, and three had non-significant increases in screening SSLDR (Table 1). Change in mean withdrawal time was positively correlated with change in SSLDR (Spearman’s rank rho = 1, P = 0.02, Figure 1). There was a non-significant increase in group screening ADR at week 23 (54.7% vs 49.3%, P = 0.28). Two endoscopists had non-significant increases in screening ADR but not SSLDR.
Discussion: Quarterly scorecards did not significantly change SSLDR by week 23, although some endoscopists had numeric increases in SSLDR, ADR, or both. Increased mean withdrawal time after feedback may associate with improvement in SSLDR. Given the infrequent detection of SSLs in an above-average SSLDR group, a larger sample size and longer timeframe are likely needed to determine SSLDR changes. Further evaluation is required to determine whether significant improvements can be achieved with extended intervention.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Brian E.. White, MD, Richard M.. Wu, MD, MPH. P3839 - Evaluation of the Impact of Endoscopic Education With Endoscopist-Specific Scorecard Feedback on the Sessile Serrated Lesion Detection Rate (SSLDR), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Pennsylvania Health System, Philadelphia, PA
Introduction: The adenoma detection rate (ADR) is a validated quality metric that associates with reduced colorectal cancer risk and has been shown to increase with endoscopist scorecard feedback. The sessile serrated lesion detection rate (SSLDR) is an emerging quality metric sharing a similar inverse association with interval CRC risk, independent of ADR. A new proposed SSLDR benchmark (6%) makes measuring and quality improvement of SSLDR timely and poignant. This study aims to evaluate the impact of endoscopist-specific scorecard feedback with a simultaneous SSL endoscopic educational component on the SSLDR, which is understudied to date.
Methods: This is an interim analysis of a prospective quality improvement project. Baseline SSLDRs and ADRs were obtained over a thirteen-week period using a natural language processing-based tool and validated with manual chart review. Endoscopists were issued scorecards detailing their individual and group quality metrics along with evidence-based practice tips for improving SSLDR at weeks 0 and 13. Baseline and intervention period (weeks 1-23) SSLDR and ADR were compared with chi-squared test. Spearman's rank test was used to assess correlation between quality metrics. Statistical analysis was performed using RStudio 2024.04.1.
Results: 96 SSLs were detected over 1118 total colonoscopies. Among the group, there were no significant changes in total or screening SSLDR at week 23 compared to baseline (9.5% vs 8.7%, P = 0.65 and 9.4% vs 7.9%, P = 0.69). Two of five endoscopists had non-significant increases in total SSLDR at week 23, and three had non-significant increases in screening SSLDR (Table 1). Change in mean withdrawal time was positively correlated with change in SSLDR (Spearman’s rank rho = 1, P = 0.02, Figure 1). There was a non-significant increase in group screening ADR at week 23 (54.7% vs 49.3%, P = 0.28). Two endoscopists had non-significant increases in screening ADR but not SSLDR.
Discussion: Quarterly scorecards did not significantly change SSLDR by week 23, although some endoscopists had numeric increases in SSLDR, ADR, or both. Increased mean withdrawal time after feedback may associate with improvement in SSLDR. Given the infrequent detection of SSLs in an above-average SSLDR group, a larger sample size and longer timeframe are likely needed to determine SSLDR changes. Further evaluation is required to determine whether significant improvements can be achieved with extended intervention.
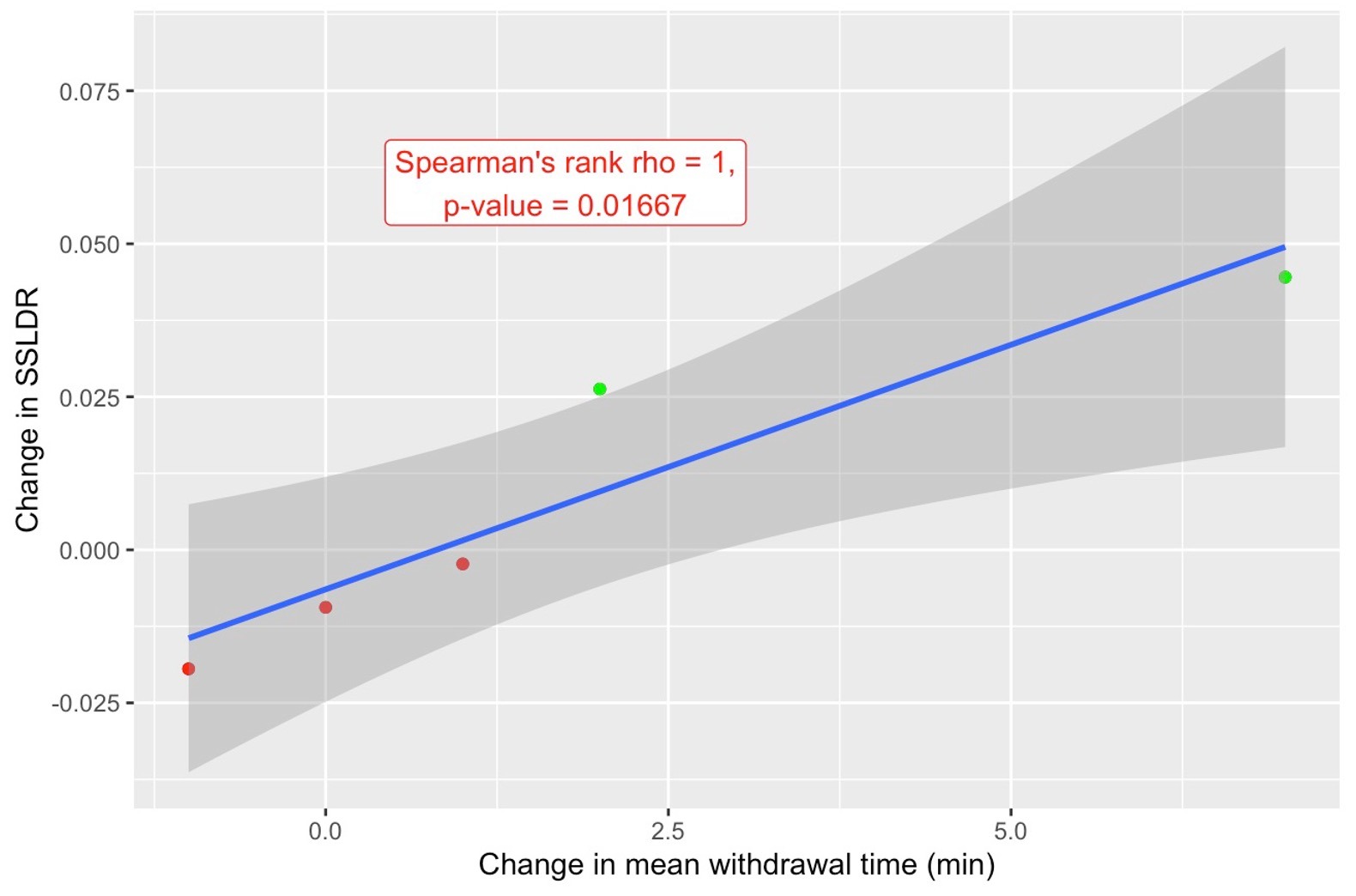
Figure: Figure 1. Change in Sessile Serrated Lesion Detection Rate (SSLDR) vs Change in Mean Withdrawal Time
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Brian White indicated no relevant financial relationships.
Richard Wu indicated no relevant financial relationships.
Brian E.. White, MD, Richard M.. Wu, MD, MPH. P3839 - Evaluation of the Impact of Endoscopic Education With Endoscopist-Specific Scorecard Feedback on the Sessile Serrated Lesion Detection Rate (SSLDR), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
