Tuesday Poster Session
Category: Colon
P3769 - Management of Complicated Crohn's Disease: Endoscopic Closure of Colo-Colonic Fistula With Concurrent Colovesical Fistula
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Kranthi K. Mandava, MD
Rutgers New Jersey Medical School
Highland Park, NJ
Presenting Author(s)
Kranthi Mandava, MD, Michael Bebawy, DO, Ritik M. Goyal, MBBS, Yazan Abboud, MD, Navid Radfar, DO, Kaveh Hajifathalian, MD, Ahmed Al-Khazraji, MD
Rutgers New Jersey Medical School, Newark, NJ
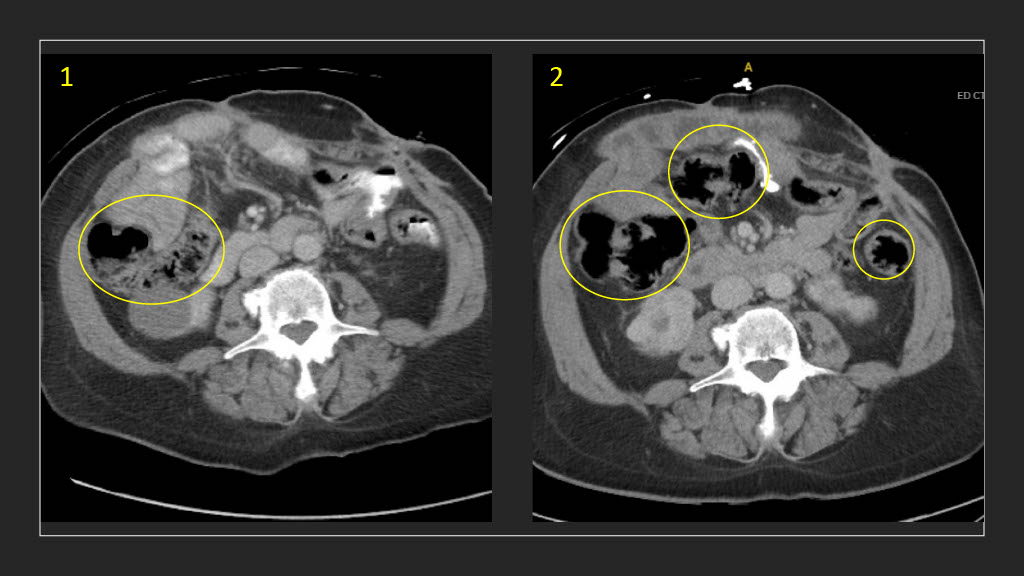
Introduction: A well-described sequalae of Crohn's disease (CD) is the development of fistulas between various parts of the digestive tract, with the most common being perianal fistulas. A less commonly observed phenomena in CD is a colovesical fistula, which occurs in 5-7% of cases. We present a case of a patient with a known colovesical fistula who later developed new fistulas in the aftermath of the surgical repairs performed to correct his intestinal disease.
Case Description/Methods: The patient is a 61-year-old male with an extensive history of CD c/b diverticulosis s/p sigmoid resection and loop colostomy in 2009, later c/b colovesical and enterocutaneous fistulas. He underwent exploratory laparotomy, lysis of adhesions and a small bowel resection for his enterocutaneous/perianal fistula tracts and scrotal abscesses and was left with a colostomy and urethra-scrotal fistula. He initially presented to the hospital after an opiate overdose, and briefly required upgrade to ICU on admission. GI was consulted for evaluation of his extensive fistulas, due to stool being expressed from his urethra. The patient underwent his first colonoscopy on day 10, where a new colo-colonic fistula was visualized but was not closed due to large stool burden despite bowel preparation; a PEG tube was placed at the fistula site to lavage the stool. On day 17 the patient went for repeat colonoscopy, having undergone an extensive 3-day bowel prep. The fistula was sutured around the PEG tube and the tube was set to low intermittent suction. In the aftermath of his surgical intervention, the patient denied any fecal matter present in his urine or any PEG site drainage. He drained 150 cc of light brown fluid without any overt feculent matter from his PEG tube; the remainder of his bowel movements occurred only from his anus. He was discharged with plans for outpatient general surgery evaluation of his remaining fistulas.
Discussion: Complex fistulas pose a substantial burden on patients who suffer from CD, with perianal fistulas accounting for 70-80% of cases. In addition to decreasing quality of life, the fistula burden may also increase healthcare resource costs. One area that can be explored to mitigate these costs is identifying an ideal bowel prep that would provide adequate visibility. Additionally, utilizing less invasive techniques for fistula closure would prove beneficial in patients with complicated fistulas, given that current surgical treatments predispose patient to developing further complications.
Disclosures:
Kranthi Mandava, MD, Michael Bebawy, DO, Ritik M. Goyal, MBBS, Yazan Abboud, MD, Navid Radfar, DO, Kaveh Hajifathalian, MD, Ahmed Al-Khazraji, MD. P3769 - Management of Complicated Crohn's Disease: Endoscopic Closure of Colo-Colonic Fistula With Concurrent Colovesical Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Rutgers New Jersey Medical School, Newark, NJ
Introduction: A well-described sequalae of Crohn's disease (CD) is the development of fistulas between various parts of the digestive tract, with the most common being perianal fistulas. A less commonly observed phenomena in CD is a colovesical fistula, which occurs in 5-7% of cases. We present a case of a patient with a known colovesical fistula who later developed new fistulas in the aftermath of the surgical repairs performed to correct his intestinal disease.
Case Description/Methods: The patient is a 61-year-old male with an extensive history of CD c/b diverticulosis s/p sigmoid resection and loop colostomy in 2009, later c/b colovesical and enterocutaneous fistulas. He underwent exploratory laparotomy, lysis of adhesions and a small bowel resection for his enterocutaneous/perianal fistula tracts and scrotal abscesses and was left with a colostomy and urethra-scrotal fistula. He initially presented to the hospital after an opiate overdose, and briefly required upgrade to ICU on admission. GI was consulted for evaluation of his extensive fistulas, due to stool being expressed from his urethra. The patient underwent his first colonoscopy on day 10, where a new colo-colonic fistula was visualized but was not closed due to large stool burden despite bowel preparation; a PEG tube was placed at the fistula site to lavage the stool. On day 17 the patient went for repeat colonoscopy, having undergone an extensive 3-day bowel prep. The fistula was sutured around the PEG tube and the tube was set to low intermittent suction. In the aftermath of his surgical intervention, the patient denied any fecal matter present in his urine or any PEG site drainage. He drained 150 cc of light brown fluid without any overt feculent matter from his PEG tube; the remainder of his bowel movements occurred only from his anus. He was discharged with plans for outpatient general surgery evaluation of his remaining fistulas.
Discussion: Complex fistulas pose a substantial burden on patients who suffer from CD, with perianal fistulas accounting for 70-80% of cases. In addition to decreasing quality of life, the fistula burden may also increase healthcare resource costs. One area that can be explored to mitigate these costs is identifying an ideal bowel prep that would provide adequate visibility. Additionally, utilizing less invasive techniques for fistula closure would prove beneficial in patients with complicated fistulas, given that current surgical treatments predispose patient to developing further complications.
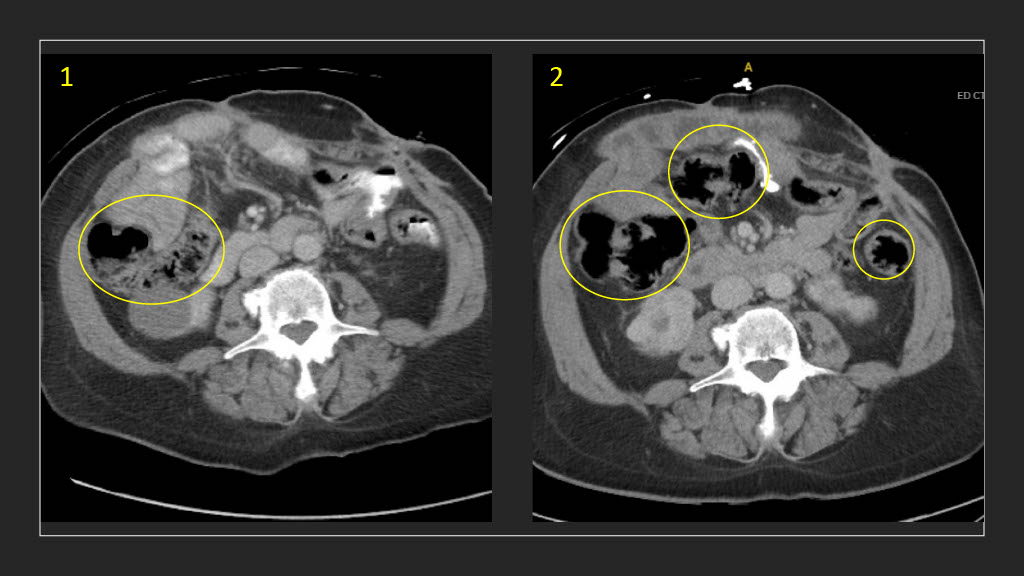
Figure: 1. Patient's colovesicular fistula on previous admission
2. Patient's colovesicular fistula during current admission, with new colo-colonic fistula
2. Patient's colovesicular fistula during current admission, with new colo-colonic fistula
Disclosures:
Kranthi Mandava indicated no relevant financial relationships.
Michael Bebawy indicated no relevant financial relationships.
Ritik Goyal indicated no relevant financial relationships.
Yazan Abboud indicated no relevant financial relationships.
Navid Radfar indicated no relevant financial relationships.
Kaveh Hajifathalian indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Kranthi Mandava, MD, Michael Bebawy, DO, Ritik M. Goyal, MBBS, Yazan Abboud, MD, Navid Radfar, DO, Kaveh Hajifathalian, MD, Ahmed Al-Khazraji, MD. P3769 - Management of Complicated Crohn's Disease: Endoscopic Closure of Colo-Colonic Fistula With Concurrent Colovesical Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
