Tuesday Poster Session
Category: Colon
P3772 - Never Too Late for PTLD: Colonic Ulcers 11 Years After Lung Transplant
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Usman Ansari, DO
Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Usman Ansari, DO, Tiffany Sheu, MD, Mary R. Schwartz, MD, Gulchin Ergun, MD
Houston Methodist Hospital, Houston, TX
Introduction: Post transplant lymphoproliferative disease (PTLD) of the gastrointestinal (GI) tract is a rare but serious complication of chronic immune suppressive therapy (IST) in solid organ transplant (SOT) and hematopoietic stem cell transplant (HCT) recipients. Risk factors include degree and type of IST, Epstein Barr Virus (EBV) serostatus of the recipient, and time post-transplant. The greatest risk of PTLD development is within the first year of HCT and within five years of SOT. Here we present an interesting case of PTLD.
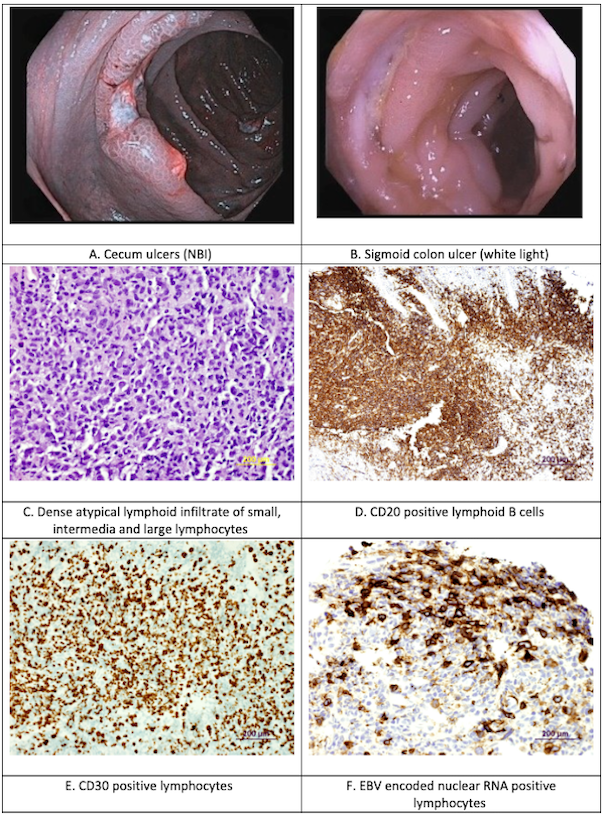
Case Description/Methods: 68-year-old male with prior history of double lung transplant in 2012, aortic stenosis, transient ischemic attack on aspirin and clopidogrel, chronic kidney disease, and recently diagnosed iron deficiency anemia (IDA) was admitted to the hospital with melena, cough, fevers, night sweats, unintentional weight loss, and progressive fatigue. He was diagnosed with acute cellular rejection of his lung graft two months prior and was treated with high dose corticosteroids and anti-thymocyte globulin. A computed tomography (CT) of the chest/abdomen/pelvis showed numerous pulmonary nodules involving all lobes and multiple bilobar hepatic lesions. Esophagogastroduodenoscopy (EGD) was normal. Colonoscopy revealed multiple deep colonic ulcers spanning from the rectum to the cecum, largest approximately 30 mm. Pathology from stomach, duodenum, colon, and liver biopsies showed EBV positive atypical B cells in lymphoid aggregates. The constellation of findings was consistent with a diagnosis of Post Transplant Lymphoproliferative Disease (PTLD). EBV polymerase chain reaction (PCR) was 7,450. Azathioprine was immediately discontinued, while tacrolimus and prednisone dosing were reduced. After 6 weeks of rituximab, positron emission tomography (PET)-CT revealed interval complete metabolic response. Follow-up endoscopies showed healed colonic ulcers; segmental biopsies showed no residual EBV positive B cell tissue. EBV PCR no longer is detected. Clinically the patient’s bleeding, B symptoms, and IDA have resolved.
Discussion: This case highlights the importance of keeping a broad differential for colonic ulcers in a SOT recipient, irrespective of time from transplant. To our knowledge, PTLD has been associated with colon ulcers up to 7 years out from time of SOT in the literature. This patient was 11 years outside of his SOT. This patient, however, did respond to conventional treatment strategies including IST reduction and rituximab therapy.
Disclosures:
Usman Ansari, DO, Tiffany Sheu, MD, Mary R. Schwartz, MD, Gulchin Ergun, MD. P3772 - Never Too Late for PTLD: Colonic Ulcers 11 Years After Lung Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Houston Methodist Hospital, Houston, TX
Introduction: Post transplant lymphoproliferative disease (PTLD) of the gastrointestinal (GI) tract is a rare but serious complication of chronic immune suppressive therapy (IST) in solid organ transplant (SOT) and hematopoietic stem cell transplant (HCT) recipients. Risk factors include degree and type of IST, Epstein Barr Virus (EBV) serostatus of the recipient, and time post-transplant. The greatest risk of PTLD development is within the first year of HCT and within five years of SOT. Here we present an interesting case of PTLD.
Case Description/Methods: 68-year-old male with prior history of double lung transplant in 2012, aortic stenosis, transient ischemic attack on aspirin and clopidogrel, chronic kidney disease, and recently diagnosed iron deficiency anemia (IDA) was admitted to the hospital with melena, cough, fevers, night sweats, unintentional weight loss, and progressive fatigue. He was diagnosed with acute cellular rejection of his lung graft two months prior and was treated with high dose corticosteroids and anti-thymocyte globulin. A computed tomography (CT) of the chest/abdomen/pelvis showed numerous pulmonary nodules involving all lobes and multiple bilobar hepatic lesions. Esophagogastroduodenoscopy (EGD) was normal. Colonoscopy revealed multiple deep colonic ulcers spanning from the rectum to the cecum, largest approximately 30 mm. Pathology from stomach, duodenum, colon, and liver biopsies showed EBV positive atypical B cells in lymphoid aggregates. The constellation of findings was consistent with a diagnosis of Post Transplant Lymphoproliferative Disease (PTLD). EBV polymerase chain reaction (PCR) was 7,450. Azathioprine was immediately discontinued, while tacrolimus and prednisone dosing were reduced. After 6 weeks of rituximab, positron emission tomography (PET)-CT revealed interval complete metabolic response. Follow-up endoscopies showed healed colonic ulcers; segmental biopsies showed no residual EBV positive B cell tissue. EBV PCR no longer is detected. Clinically the patient’s bleeding, B symptoms, and IDA have resolved.
Discussion: This case highlights the importance of keeping a broad differential for colonic ulcers in a SOT recipient, irrespective of time from transplant. To our knowledge, PTLD has been associated with colon ulcers up to 7 years out from time of SOT in the literature. This patient was 11 years outside of his SOT. This patient, however, did respond to conventional treatment strategies including IST reduction and rituximab therapy.
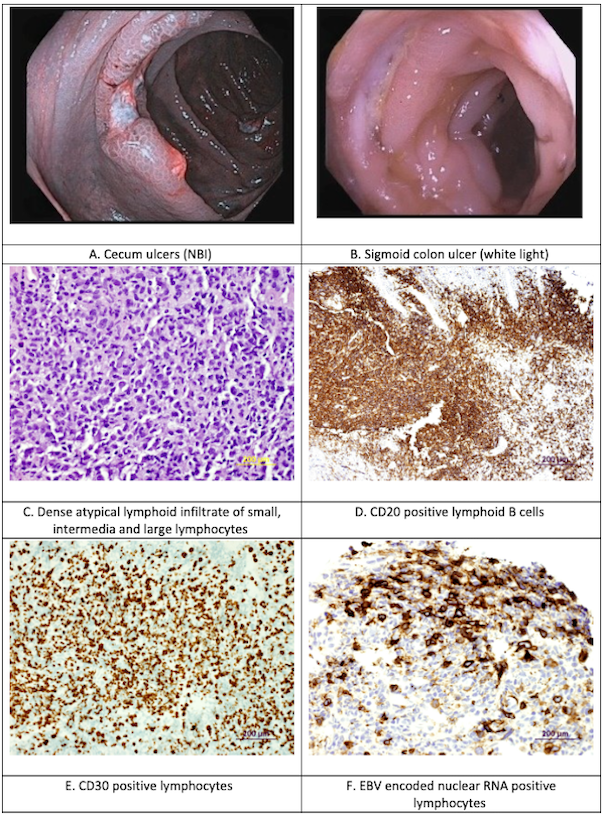
Figure: Figure 1: Colonoscopy and Histology Images
Disclosures:
Usman Ansari indicated no relevant financial relationships.
Tiffany Sheu indicated no relevant financial relationships.
Mary Schwartz indicated no relevant financial relationships.
Gulchin Ergun indicated no relevant financial relationships.
Usman Ansari, DO, Tiffany Sheu, MD, Mary R. Schwartz, MD, Gulchin Ergun, MD. P3772 - Never Too Late for PTLD: Colonic Ulcers 11 Years After Lung Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
