Tuesday Poster Session
Category: Colon
P3782 - Streptococcal Proctitis in a Healthy Adult Female Following Scarlet Fever
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- ER
Elizabeth Reznik, MD
New York-Presbyterian/Weill Cornell
New York, NY
Presenting Author(s)
Elizabeth Reznik, MD1, Sybil Olmo, NP2, David Wan, MD2
1New York-Presbyterian/Weill Cornell, New York, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY
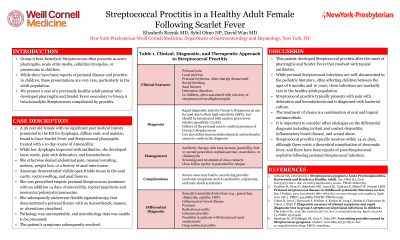
Introduction: Group A beta-hemolytic Streptococcus often presents as acute pharyngitis, acute otitis media, cellulitis/erysipelas, or pneumonia in children. While there have been reports of perianal disease and proctitis in children, these presentations are very rare, particularly in the adult population. We present a case of a previously healthy adult patient who developed pharyngitis and Scarlet Fever secondary to Group A beta-hemolytic Streptococcus complicated by proctitis.
Case Description/Methods: A 36 year old female with no significant past medical history presented to the ED for dysphagia, diffuse rash, and malaise, found to have Scarlet Fever and Streptococcal pharyngitis treated with a 10 day course of amoxicillin. While her dysphagia improved with antibiotics, she developed loose stools, pain with defecation, and hematochezia. She otherwise denied abdominal pain, nausea/vomiting, melena, weight loss, or a history of anal intercourse. She was prescribed empiric perianal Streptococcus treatment with mupirocin and neomycin/polymyxin/pramoxine. She subsequently underwent flexible sigmoidoscopy that demonstrated normal rectal mucosa with no hemorrhoids, masses, or ulcerations visualized. Pathology was unremarkable, and microbiology data was sent, but unfortunately, unable to be processed. The patient’s symptoms subsequently resolved with topical antibiotics.
Discussion: This patient developed Streptococcal proctitis after the onset of pharyngitis and Scarlet Fever that resolved with topical antibiotics. While perianal Streptococcal infections are well-documented in the pediatric literature, often affecting children between the ages of 6 months and 10 years, these infections are markedly rare in the healthy adult population. Streptococcal proctitis typically presents with pain with defecation and hematochezia and is diagnosed with bacterial culture. The treatment of choice is a combination of oral and topical antimicrobials. It is important to consider other etiologies on the differential diagnosis including irritant and contact dermatitis, inflammatory bowel disease, and sexual abuse. Streptococcal proctitis typically resolves within 14-21 days, although there exists a theoretical complication of rheumatic fever, and there have been reports of post-Streptococcal nephritis following perianal Streptococcal infection.
Disclosures:
Elizabeth Reznik, MD1, Sybil Olmo, NP2, David Wan, MD2. P3782 - Streptococcal Proctitis in a Healthy Adult Female Following Scarlet Fever, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian/Weill Cornell, New York, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Group A beta-hemolytic Streptococcus often presents as acute pharyngitis, acute otitis media, cellulitis/erysipelas, or pneumonia in children. While there have been reports of perianal disease and proctitis in children, these presentations are very rare, particularly in the adult population. We present a case of a previously healthy adult patient who developed pharyngitis and Scarlet Fever secondary to Group A beta-hemolytic Streptococcus complicated by proctitis.
Case Description/Methods: A 36 year old female with no significant past medical history presented to the ED for dysphagia, diffuse rash, and malaise, found to have Scarlet Fever and Streptococcal pharyngitis treated with a 10 day course of amoxicillin. While her dysphagia improved with antibiotics, she developed loose stools, pain with defecation, and hematochezia. She otherwise denied abdominal pain, nausea/vomiting, melena, weight loss, or a history of anal intercourse. She was prescribed empiric perianal Streptococcus treatment with mupirocin and neomycin/polymyxin/pramoxine. She subsequently underwent flexible sigmoidoscopy that demonstrated normal rectal mucosa with no hemorrhoids, masses, or ulcerations visualized. Pathology was unremarkable, and microbiology data was sent, but unfortunately, unable to be processed. The patient’s symptoms subsequently resolved with topical antibiotics.
Discussion: This patient developed Streptococcal proctitis after the onset of pharyngitis and Scarlet Fever that resolved with topical antibiotics. While perianal Streptococcal infections are well-documented in the pediatric literature, often affecting children between the ages of 6 months and 10 years, these infections are markedly rare in the healthy adult population. Streptococcal proctitis typically presents with pain with defecation and hematochezia and is diagnosed with bacterial culture. The treatment of choice is a combination of oral and topical antimicrobials. It is important to consider other etiologies on the differential diagnosis including irritant and contact dermatitis, inflammatory bowel disease, and sexual abuse. Streptococcal proctitis typically resolves within 14-21 days, although there exists a theoretical complication of rheumatic fever, and there have been reports of post-Streptococcal nephritis following perianal Streptococcal infection.
Disclosures:
Elizabeth Reznik indicated no relevant financial relationships.
Sybil Olmo indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Elizabeth Reznik, MD1, Sybil Olmo, NP2, David Wan, MD2. P3782 - Streptococcal Proctitis in a Healthy Adult Female Following Scarlet Fever, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
