Tuesday Poster Session
Category: Colon
P3783 - Acute Colonic Pseudo-Obstruction: A Case Highlighting Pitfalls in Imaging
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RS
Rachel Schwartz, DO
Texas Institute for Graduate Medical Education and Research San Antonio
San Antonio, TX
Presenting Author(s)
Rachel Schwartz, DO1, Ryan Sanchez, DO2, Patrick Snyder, MD2
1Texas Institute for Graduate Medical Education and Research San Antonio, San Antonio, TX; 2University of Texas Health San Antonio, San Antonio, TX
Introduction: The etiologies of acute colonic dilation can be broadly divided into mechanical and functional causes. Acute colonic pseudo-obstruction (ACPO, or Ogilvie’s Syndrome) is marked by dilation of the colon in absence of an obstructing lesion. We present an interesting case of ACPO with imaging findings that emphasize this distinction.
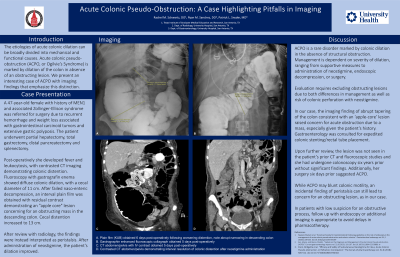
Case Description/Methods: A 47-year-old female with history of MEN1 and associated Zollinger-Ellison syndrome was referred for surgery due to recurrent hemorrhage and weight loss associated with gastrointestinal carcinoid tumors and extensive gastric polyposis. The patient underwent partial hepatectomy, total gastrectomy, distal pancreatectomy and splenectomy. Post-operatively she developed fever and leukocytosis, with contrasted CT imaging demonstrating colonic distention. Fluoroscopy with gastrografin enema showed diffuse colonic dilation, with a cecal diameter of 11 cm. After failed naso-enteric decompression, an interval plain film was obtained with residual contrast demonstrating an "apple core" lesion concerning for an obstructing mass in the descending colon. Cecal distention increased to 13 cm. After review with radiology, the findings were instead interpreted as peristalsis. After administration of neostigmine, the patient’s dilation improved.
Discussion: ACPO is a rare disorder marked by colonic dilation in the absence of structural obstruction. Management is dependent on severity of dilation, ranging from supportive measures to administration of neostigmine, endoscopic decompression, or surgery. Evaluation requires excluding obstructing lesions due to both differences in management as well as risk of colonic perforation with neostigmine. In our case, the imaging finding of abrupt tapering of the colon consistent with an ‘apple-core’ lesion raised concern for acute obstruction due to a mass, especially given the patient’s history. Gastroenterology was consulted for expedited colonic stenting/rectal tube placement. Upon further review, the lesion was not seen in the patient’s prior CT and fluoroscopic studies and she had undergone colonoscopy six years prior without significant findings. Additionally, her surgery six days prior suggested ACPO. While ACPO may blunt colonic motility, an incidental finding of peristalsis can still lead to concern for an obstructing lesion, as in our case. In patients with low suspicion for an obstructive process, follow up with endoscopy or additional imaging is appropriate to avoid delays in pharmacotherapy.
Disclosures:
Rachel Schwartz, DO1, Ryan Sanchez, DO2, Patrick Snyder, MD2. P3783 - Acute Colonic Pseudo-Obstruction: A Case Highlighting Pitfalls in Imaging, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Texas Institute for Graduate Medical Education and Research San Antonio, San Antonio, TX; 2University of Texas Health San Antonio, San Antonio, TX
Introduction: The etiologies of acute colonic dilation can be broadly divided into mechanical and functional causes. Acute colonic pseudo-obstruction (ACPO, or Ogilvie’s Syndrome) is marked by dilation of the colon in absence of an obstructing lesion. We present an interesting case of ACPO with imaging findings that emphasize this distinction.
Case Description/Methods: A 47-year-old female with history of MEN1 and associated Zollinger-Ellison syndrome was referred for surgery due to recurrent hemorrhage and weight loss associated with gastrointestinal carcinoid tumors and extensive gastric polyposis. The patient underwent partial hepatectomy, total gastrectomy, distal pancreatectomy and splenectomy. Post-operatively she developed fever and leukocytosis, with contrasted CT imaging demonstrating colonic distention. Fluoroscopy with gastrografin enema showed diffuse colonic dilation, with a cecal diameter of 11 cm. After failed naso-enteric decompression, an interval plain film was obtained with residual contrast demonstrating an "apple core" lesion concerning for an obstructing mass in the descending colon. Cecal distention increased to 13 cm. After review with radiology, the findings were instead interpreted as peristalsis. After administration of neostigmine, the patient’s dilation improved.
Discussion: ACPO is a rare disorder marked by colonic dilation in the absence of structural obstruction. Management is dependent on severity of dilation, ranging from supportive measures to administration of neostigmine, endoscopic decompression, or surgery. Evaluation requires excluding obstructing lesions due to both differences in management as well as risk of colonic perforation with neostigmine. In our case, the imaging finding of abrupt tapering of the colon consistent with an ‘apple-core’ lesion raised concern for acute obstruction due to a mass, especially given the patient’s history. Gastroenterology was consulted for expedited colonic stenting/rectal tube placement. Upon further review, the lesion was not seen in the patient’s prior CT and fluoroscopic studies and she had undergone colonoscopy six years prior without significant findings. Additionally, her surgery six days prior suggested ACPO. While ACPO may blunt colonic motility, an incidental finding of peristalsis can still lead to concern for an obstructing lesion, as in our case. In patients with low suspicion for an obstructive process, follow up with endoscopy or additional imaging is appropriate to avoid delays in pharmacotherapy.
Figure: A. Plain film (KUB) obtained 6 days post-operatively following worsening distention, note abrupt narrowing in descending colon. B. Gastrographin enhanced fluoroscopic collagraph obtained 5 days post-operatively. C. CT abdomen/pelvis with IV contrast obtained 5 days post-operatively.
Disclosures:
Rachel Schwartz indicated no relevant financial relationships.
Ryan Sanchez indicated no relevant financial relationships.
Patrick Snyder indicated no relevant financial relationships.
Rachel Schwartz, DO1, Ryan Sanchez, DO2, Patrick Snyder, MD2. P3783 - Acute Colonic Pseudo-Obstruction: A Case Highlighting Pitfalls in Imaging, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
