Tuesday Poster Session
Category: Colon
P3719 - Multi-Station Portal Hypertensive Polyps: A Unique Complication of Portal Hypertension
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Suvithan Rajadurai, MD
Brown Medicine/Lifespan
Providence, RI
Presenting Author(s)
Suvithan Rajadurai, MD1, Hanna Wang, 2, Yousef Elfanagely, MD2, Syed Quadri, MD1, Bryce Perler, MD3
1Brown Medicine/Lifespan, Providence, RI; 2Brown University, Providence, RI; 3Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction: A major complication of cirrhosis is increased portal pressure leading to portal hypertension (PH). Structural changes to the liver parenchyma, low nitric oxide production, and high splanchnic blood flow contribute to PH. Sequelae of PH involve formation of varices, gastropathy, enteropathy, and even thrombocytopenia. Reports even show polyposis secondary to PH with gastric polyps being most common. It is far rarer for patients to present with these polyps in other sections of the gastrointestinal (GI) tract. We describe a patient with several polyps throughout their GI tract in the setting of portal hypertensive polyposis (PHP).
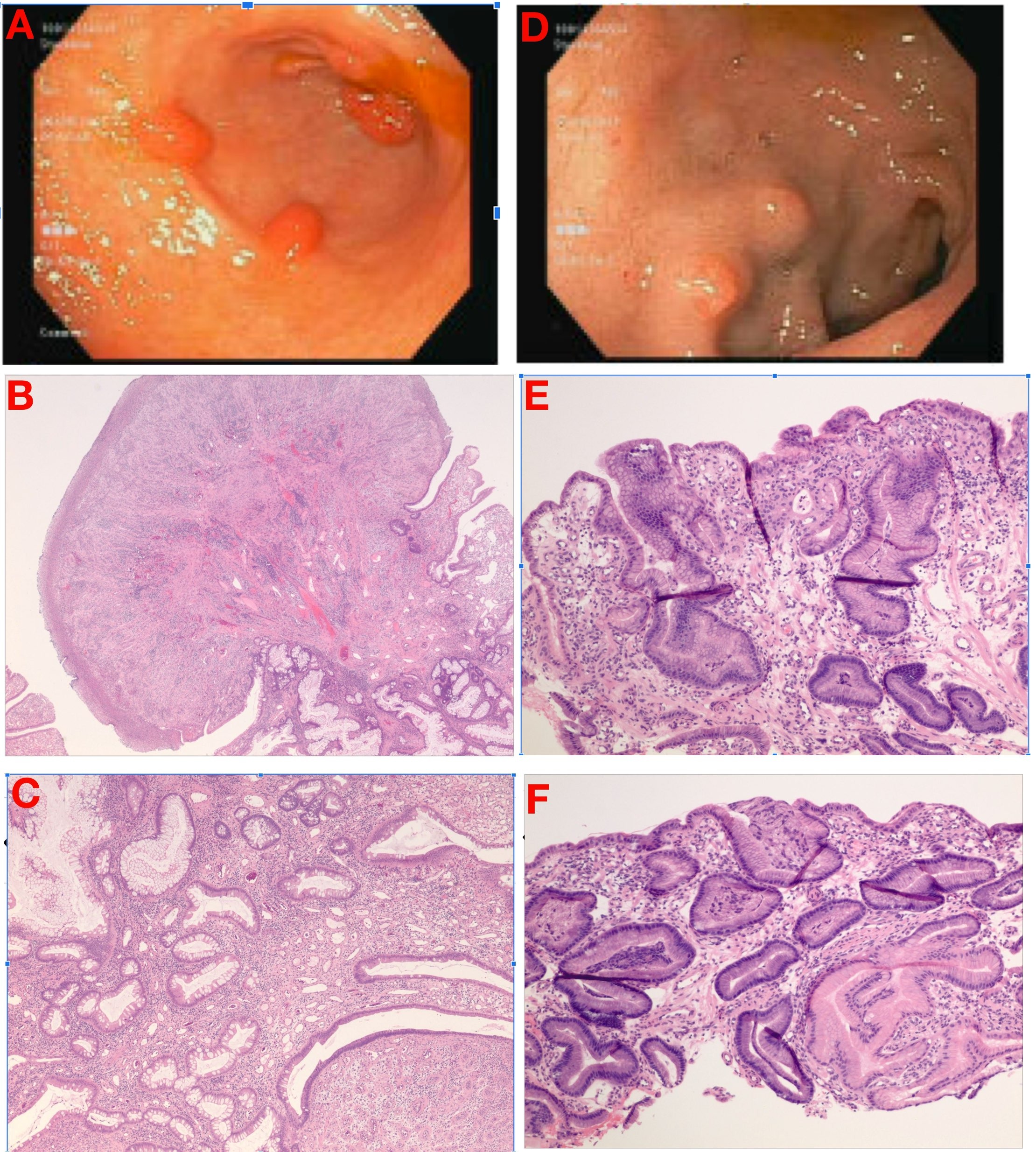
Case Description/Methods: A 19-year-old female with a history of congenital PH with portal vein thrombosis complicated by ascites, esophageal varices, splenomegaly presented with diarrhea and weight loss for which endoscopy was performed. Colonoscopy revealed 6 < 1cm semi-pedunculated polyps in the recto-sigmoid colon with 1 in the transverse. Upper endoscopy showed 4 large varices in the lower third of the esophagus, 5 pedunculated and sessile polyps in the gastric antrum, and 6 duodenal polyps all < 1cm. Biopsy demonstrated telangiectasia, variable smooth muscle extension into the mucosa and hyperplastic change noted to be features seen in polypoid lesions of the GI tract from PH. Several repeat endoscopies demonstrated additional similar lesions histologically despite prior removal. The patient has continued to suffer from complications of PH including ischemic bowel from acute thrombosis of the superior mesenteric vein leading to small bowel resection.
Discussion: Lesions can be identified on a microscopic level where hyperplastic changes and vascular ectasias that extend into the lamina propria which distinguish them from inflammatory polyps, there is no clear diagnostic criteria for individual polyps or PHP. Pathogenesis of these polyps is not clear; some theories suggest that high portal pressure leads to angiogenesis and growth. While research surrounding gastric PHPs is mostly limited, literature on duodenal and colonic PHPs is even rarer likely due to unfamiliarity. Little is known about the risks and benefits of resection as some studies have shown that despite high recurrence rates, they often do not transform into malignancy. Studies are needed to determine if the burden of PHPs pose an increased risk in terms of cirrhosis complications or malignancy and guidelines regarding management of these polyps, especially in young patients with cirrhosis.
Disclosures:
Suvithan Rajadurai, MD1, Hanna Wang, 2, Yousef Elfanagely, MD2, Syed Quadri, MD1, Bryce Perler, MD3. P3719 - Multi-Station Portal Hypertensive Polyps: A Unique Complication of Portal Hypertension, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brown Medicine/Lifespan, Providence, RI; 2Brown University, Providence, RI; 3Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction: A major complication of cirrhosis is increased portal pressure leading to portal hypertension (PH). Structural changes to the liver parenchyma, low nitric oxide production, and high splanchnic blood flow contribute to PH. Sequelae of PH involve formation of varices, gastropathy, enteropathy, and even thrombocytopenia. Reports even show polyposis secondary to PH with gastric polyps being most common. It is far rarer for patients to present with these polyps in other sections of the gastrointestinal (GI) tract. We describe a patient with several polyps throughout their GI tract in the setting of portal hypertensive polyposis (PHP).
Case Description/Methods: A 19-year-old female with a history of congenital PH with portal vein thrombosis complicated by ascites, esophageal varices, splenomegaly presented with diarrhea and weight loss for which endoscopy was performed. Colonoscopy revealed 6 < 1cm semi-pedunculated polyps in the recto-sigmoid colon with 1 in the transverse. Upper endoscopy showed 4 large varices in the lower third of the esophagus, 5 pedunculated and sessile polyps in the gastric antrum, and 6 duodenal polyps all < 1cm. Biopsy demonstrated telangiectasia, variable smooth muscle extension into the mucosa and hyperplastic change noted to be features seen in polypoid lesions of the GI tract from PH. Several repeat endoscopies demonstrated additional similar lesions histologically despite prior removal. The patient has continued to suffer from complications of PH including ischemic bowel from acute thrombosis of the superior mesenteric vein leading to small bowel resection.
Discussion: Lesions can be identified on a microscopic level where hyperplastic changes and vascular ectasias that extend into the lamina propria which distinguish them from inflammatory polyps, there is no clear diagnostic criteria for individual polyps or PHP. Pathogenesis of these polyps is not clear; some theories suggest that high portal pressure leads to angiogenesis and growth. While research surrounding gastric PHPs is mostly limited, literature on duodenal and colonic PHPs is even rarer likely due to unfamiliarity. Little is known about the risks and benefits of resection as some studies have shown that despite high recurrence rates, they often do not transform into malignancy. Studies are needed to determine if the burden of PHPs pose an increased risk in terms of cirrhosis complications or malignancy and guidelines regarding management of these polyps, especially in young patients with cirrhosis.
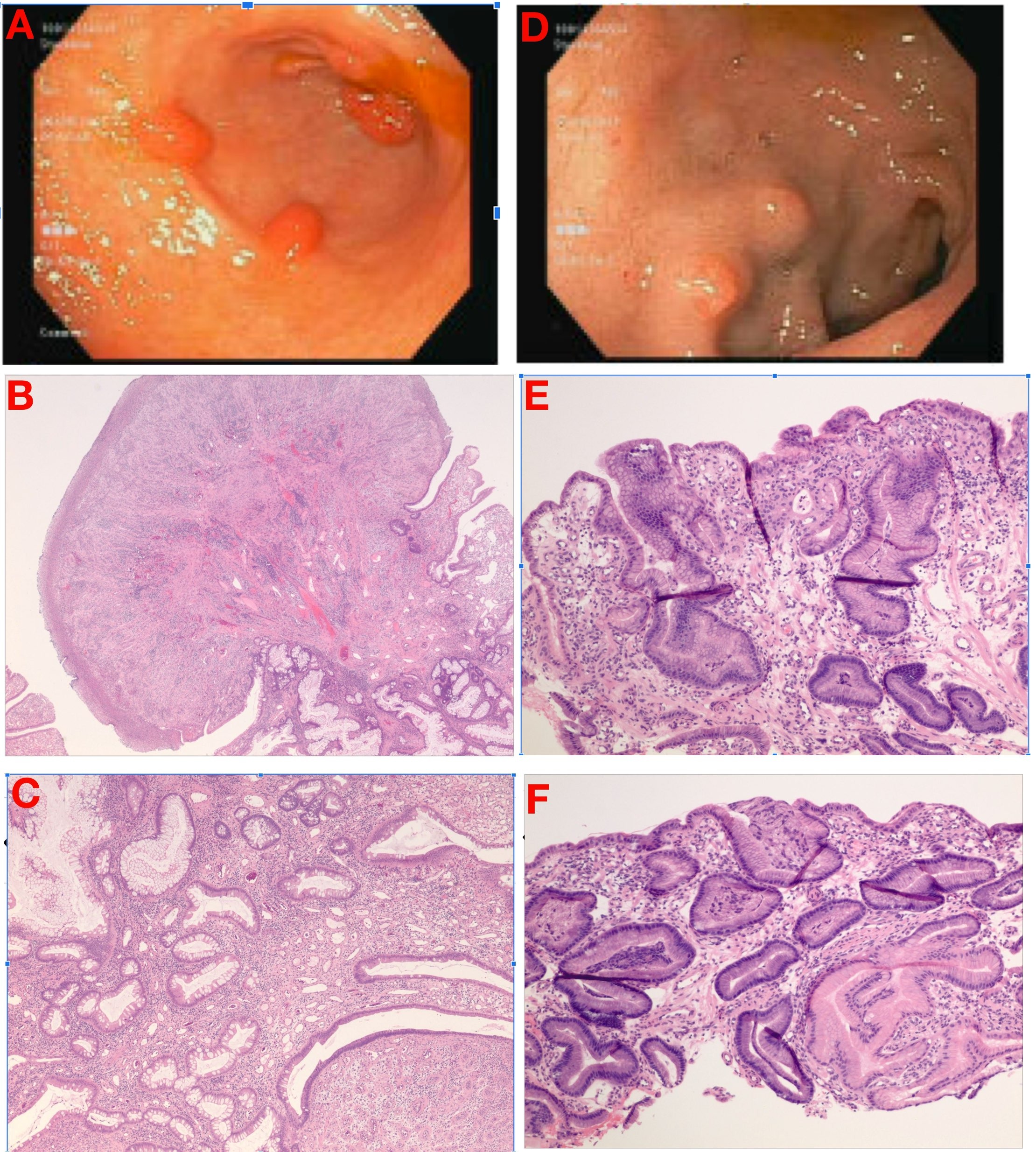
Figure: A: Hyperplastic gastric polyp B-C: H&E staining of gastric polyp demonstrating foveolar epithelium with hypertrophic features. Edematous lamina propria with lymphocytes, plasma cells and eosinophils. Smooth muscles strands extending to surface. D: Polyps present in second portion of duodenum E-F: H&E staining from sigmoid colon polyp demonstrating colonic epithelium in polypoid configuration showing various degrees of surface erosion, crypt distortion/dilation or hyperplasia, along with granulation tissue (abundant thin walled and dilated vessels surrounded by mixed neutrophilic and lymphoplasmacytic inflammation)
Disclosures:
Suvithan Rajadurai indicated no relevant financial relationships.
Hanna Wang indicated no relevant financial relationships.
Yousef Elfanagely indicated no relevant financial relationships.
Syed Quadri indicated no relevant financial relationships.
Bryce Perler indicated no relevant financial relationships.
Suvithan Rajadurai, MD1, Hanna Wang, 2, Yousef Elfanagely, MD2, Syed Quadri, MD1, Bryce Perler, MD3. P3719 - Multi-Station Portal Hypertensive Polyps: A Unique Complication of Portal Hypertension, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
