Tuesday Poster Session
Category: Colon
P3664 - Exploring the Risk of Colorectal Cancer (CRC) Metastasis in Patients With Fatty Liver: A Nationwide Analysis (2016-2020)
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Ruchir Damjibhai Paladiya, MBBS
University of Connecticut Health Center
Hartford, CT
Presenting Author(s)
Ruchir Damjibhai. Paladiya, MBBS1, Danzhu Zhao, DO2, Vikash Kumar, MD3, Aalam Sohal, MD4, Haleh Vaziri, MD2
1University of Connecticut Health Center, Hartford, CT; 2University of Connecticut Health Center, Farmington, CT; 3Creighton University School of Medicine, Brooklyn, NY; 4Creighton University School of Medicine, Seattle, WA
Introduction: Metabolic Dysfunction Associated Liver Disease (MASLD) previously known as Fatty liver (FL) is the predominant contributor to liver disease, with its prevalence increasing worldwide. Colorectal cancer (CRC) ranks the third most common cancer worldwide, bearing significant morbidity and mortality. Recent research has highlighted the impact of the fatty liver microenvironment on the rate of invasion and metastasis of CRC in in-vitro models, suggesting alterations in the tumor microenvironment (TME). The current study explores the odds of CRC metastasis in patients with FL.
Methods: National Inpatient Sample (NIS) 2016–2020 was used to identify adult patients (age >18 years) with CRC using ICD-10 codes. Patients with missing demographics and mortality data were excluded from the study. Patients were stratified into two groups based on prevalence of FL. Data were collected on patient demographics, Elixhauser Comorbidity Index (ECI), and comorbidities. The outcomes studied were rates of liver, gastrointestinal (GI), non-GI, and lymphoid metastasis. A multivariate logistic regression analysis was performed to evaluate the role of FL on these outcomes.
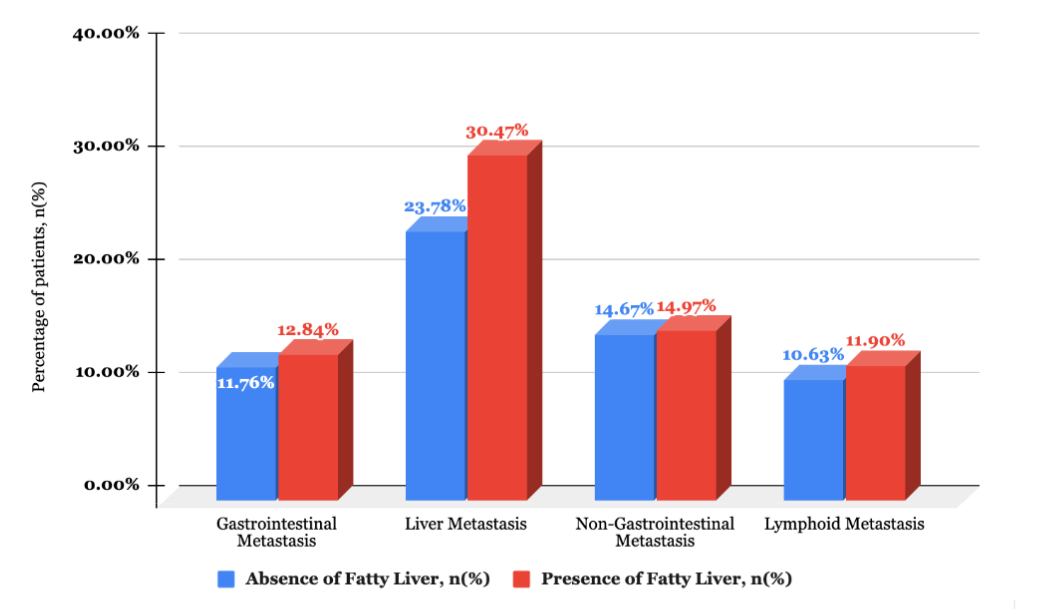
Results: Of the 814,270 patients, 35,595 (4.37%) had FL. The majority of patients in the FL group were aged >65 years (56%), male (51%) and white race (70%). There was a higher prevalence of diabetes, chronic kidney disease, coagulopathy, obesity, gastroesophageal reflux disease and obstructive sleep apnea among patients with FL. (Table 1) Patients with FL had a higher prevalence of GI metastasis (12.84% vs 11.76%, p=0.005), liver metastasis (30.47% vs 23.78%, p< 0.001), and lymphoid metastasis (11.9% vs. 10.63%, p=0.001) than those who did not have FL (Figure 1). After adjusting for confounding factors (patient demographics, ECI and comorbidities), patients with FL had higher odds of having total metastasis (aOR-1.24, 95% CI- 1.18-1.30, p< 0.001), GI metastasis (aOR-1.08, 95% CI-1-1.16, p=0.030), liver metastasis (aOR-1.38, 95% CI- 1.30-1.45, p< 0.001), lymphoid metastasis (aOR-1.12, 95% CI-1.04-1.21, p=0.003) and in-hospital mortality (aOR-1.84, 95% CI-1.68-2.03,p< 0.001) but not non-GI metastasis (aOR-1, 95% CI-0.93-1.07, p< 0.1).
Discussion: Our study highlights that FL may be associated with higher risk of developing CRC metastasis especially metastasis to the liver. With new treatments for MASLD, it will be interesting to see whether these therapies can impact the metastasis rate in CRC. Further research is needed to confirm these findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ruchir Damjibhai. Paladiya, MBBS1, Danzhu Zhao, DO2, Vikash Kumar, MD3, Aalam Sohal, MD4, Haleh Vaziri, MD2. P3664 - Exploring the Risk of Colorectal Cancer (CRC) Metastasis in Patients With Fatty Liver: A Nationwide Analysis (2016-2020), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut Health Center, Hartford, CT; 2University of Connecticut Health Center, Farmington, CT; 3Creighton University School of Medicine, Brooklyn, NY; 4Creighton University School of Medicine, Seattle, WA
Introduction: Metabolic Dysfunction Associated Liver Disease (MASLD) previously known as Fatty liver (FL) is the predominant contributor to liver disease, with its prevalence increasing worldwide. Colorectal cancer (CRC) ranks the third most common cancer worldwide, bearing significant morbidity and mortality. Recent research has highlighted the impact of the fatty liver microenvironment on the rate of invasion and metastasis of CRC in in-vitro models, suggesting alterations in the tumor microenvironment (TME). The current study explores the odds of CRC metastasis in patients with FL.
Methods: National Inpatient Sample (NIS) 2016–2020 was used to identify adult patients (age >18 years) with CRC using ICD-10 codes. Patients with missing demographics and mortality data were excluded from the study. Patients were stratified into two groups based on prevalence of FL. Data were collected on patient demographics, Elixhauser Comorbidity Index (ECI), and comorbidities. The outcomes studied were rates of liver, gastrointestinal (GI), non-GI, and lymphoid metastasis. A multivariate logistic regression analysis was performed to evaluate the role of FL on these outcomes.
Results: Of the 814,270 patients, 35,595 (4.37%) had FL. The majority of patients in the FL group were aged >65 years (56%), male (51%) and white race (70%). There was a higher prevalence of diabetes, chronic kidney disease, coagulopathy, obesity, gastroesophageal reflux disease and obstructive sleep apnea among patients with FL. (Table 1) Patients with FL had a higher prevalence of GI metastasis (12.84% vs 11.76%, p=0.005), liver metastasis (30.47% vs 23.78%, p< 0.001), and lymphoid metastasis (11.9% vs. 10.63%, p=0.001) than those who did not have FL (Figure 1). After adjusting for confounding factors (patient demographics, ECI and comorbidities), patients with FL had higher odds of having total metastasis (aOR-1.24, 95% CI- 1.18-1.30, p< 0.001), GI metastasis (aOR-1.08, 95% CI-1-1.16, p=0.030), liver metastasis (aOR-1.38, 95% CI- 1.30-1.45, p< 0.001), lymphoid metastasis (aOR-1.12, 95% CI-1.04-1.21, p=0.003) and in-hospital mortality (aOR-1.84, 95% CI-1.68-2.03,p< 0.001) but not non-GI metastasis (aOR-1, 95% CI-0.93-1.07, p< 0.1).
Discussion: Our study highlights that FL may be associated with higher risk of developing CRC metastasis especially metastasis to the liver. With new treatments for MASLD, it will be interesting to see whether these therapies can impact the metastasis rate in CRC. Further research is needed to confirm these findings.
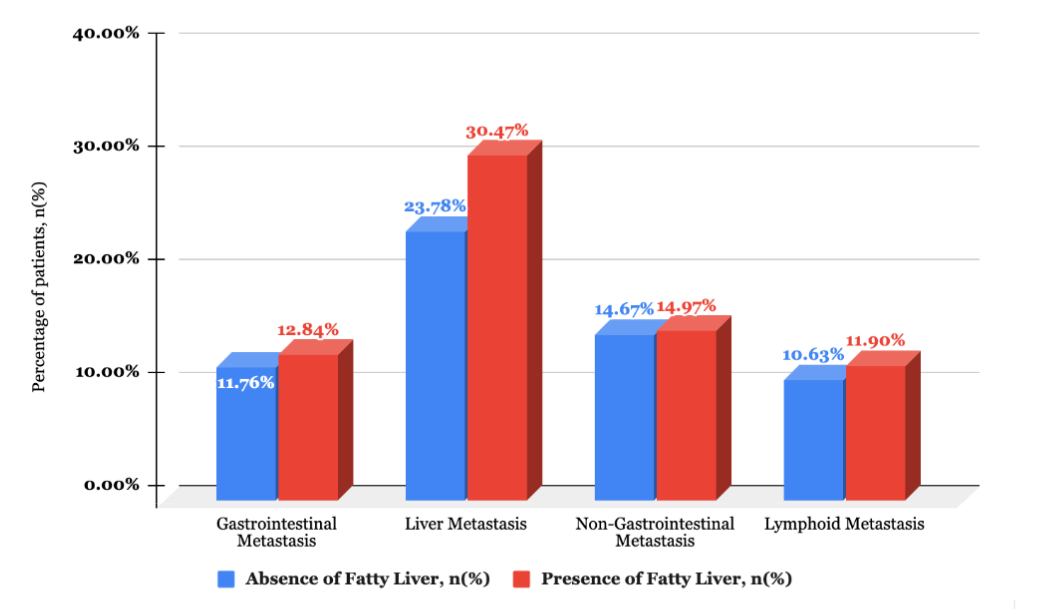
Figure: Figure 1, Association of Fatty Liver and Colorectal Cancer metastasis rate.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ruchir Paladiya indicated no relevant financial relationships.
Danzhu Zhao indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Haleh Vaziri indicated no relevant financial relationships.
Ruchir Damjibhai. Paladiya, MBBS1, Danzhu Zhao, DO2, Vikash Kumar, MD3, Aalam Sohal, MD4, Haleh Vaziri, MD2. P3664 - Exploring the Risk of Colorectal Cancer (CRC) Metastasis in Patients With Fatty Liver: A Nationwide Analysis (2016-2020), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
