Tuesday Poster Session
Category: Colon
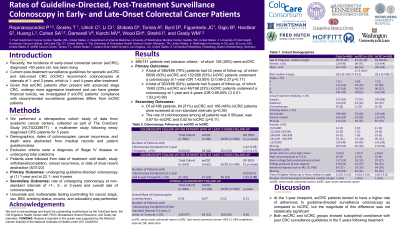
P3665 - Rates of Guideline-Directed, Post-Treatment Surveillance Colonoscopy in Early- and Late-Onset Colorectal Cancer Patients
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Pakdee Rojanasopondist, MD
University of Washington
Seattle, WA
Presenting Author(s)
Pakdee Rojanasopondist, MD1, Ted Gooley, PhD2, Cornelia Ulrich, PhD, MS3, Christopher I. Li, MD, PhD2, David Shibata, MD4, Adetunji Toriola, MD, PhD5, Doratha Byrd, PhD, MPH6, Jane C. Figueiredo, PhD7, Biljana Gigic, PhD, MSc8, Sheetal Hardikar, MBBS, PhD, MPH3, Stacey Cohen, MD2, Lyen Huang, MD, MPH9, Victoria Damerell, PhD8, Meghana V. Karchi, MPH10, Elizabeth H. Wood, MD4, Ildiko Strehli, PhD3, William M.. Grady, MD2
1University of Washington, Seattle, WA; 2Fred Hutchinson Cancer Center, Seattle, WA; 3Huntsman Cancer Institute, Salt Lake City, UT; 4University of Tennessee Health Science Center, Memphis, TN; 5Washington University School of Medicine in St. Louis, St. Louis, MO; 6Moffitt Cancer Center, Tampa, FL; 7Cedars-Sinai Medical Center, Los Angeles, CA; 8Heidelberg University Hospital, Heidelberg, Baden-Wurttemberg, Germany; 9University of Utah and Huntsman Cancer Institute, Salt Lake City, UT; 10UTHSC, Southaven, MS
Introduction: Recently, the incidence of early-onset colorectal cancer (eoCRC), diagnosed < 50 years old, has been rising. Current post-treatment surveillance guidelines for sporadic eoCRC and late-onset CRC (loCRC) recommend colonoscopies at intervals of 1- and 3-years (eg at 1- and 4-years after treatment). Given that eoCRC patients often present with advanced stage CRC, undergo more aggressive treatment and can have greater financial toxicity, we investigated if eoCRC patients’ compliance with recommended surveillance guidelines differs from loCRC patients.
Methods: We performed a retrospective cohort study of data from academic cancer centers, collected as part of a multicenter study following newly diagnosed CRC patients for 5 years. Demographics, dates of colonoscopies, cancer recurrence, and death were abstracted from medical records and patient questionnaires. Exclusion criteria were a diagnosis of Stage IV disease or undergoing total colectomy. Patients were followed until death, study withdrawal/completion, cancer recurrence, or date of most recent abstraction (8/31/23). The primary outcomes were undergoing guideline-directed colonoscopy at (1) 1-year and at (2) 1- and 4-years. Secondary outcomes were rate of undergoing colonoscopy at non-standard intervals of < 1-, 2-, or 3-years and overall rate of colonoscopies. Univariate and multivariable testing (controlling for stage, sex, BMI, smoking status, income, and education) was performed.
Results: Of 741 patients identified, 486 met inclusion criteria - of which 126 (26%) were eoCRC (Table). A total of 386/486 (79%) patients had ≥2 years of follow-up, of which 58/98 (60%) eoCRC and 152/288 (53%) loCRC patients underwent a colonoscopy at 1-year (OR 1.42,95% CI 0.86-2.37,p=0.17). A total of 263/486 (54%) patients had 5-years of follow-up, of which 15/65 (23%) eoCRC and 46/198 (23%) loCRC patients underwent a colonoscopy at 1-year and 4-years (OR 0.99,95% CI 0.51-1.93,p=0.98). Of all 486 patients, 64 (51%) eoCRC and 166 (46%) loCRC patients were screened at non-standard intervals (p=0.36). The rate of colonoscopies among all patients was 0.56/year, was 0.67 for eoCRC and 0.52 for loCRC (p=0.11).
Discussion: At the 1-year timepoint, eoCRC patients had a numerically higher rate of adherence to guideline-directed surveillance colonoscopy as compared to loCRC, but the magnitude of this difference was not large enough to be definitive. Both groups showed suboptimal compliance with post CRC surveillance guidelines in the 5 years following treatment.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Pakdee Rojanasopondist, MD1, Ted Gooley, PhD2, Cornelia Ulrich, PhD, MS3, Christopher I. Li, MD, PhD2, David Shibata, MD4, Adetunji Toriola, MD, PhD5, Doratha Byrd, PhD, MPH6, Jane C. Figueiredo, PhD7, Biljana Gigic, PhD, MSc8, Sheetal Hardikar, MBBS, PhD, MPH3, Stacey Cohen, MD2, Lyen Huang, MD, MPH9, Victoria Damerell, PhD8, Meghana V. Karchi, MPH10, Elizabeth H. Wood, MD4, Ildiko Strehli, PhD3, William M.. Grady, MD2. P3665 - Rates of Guideline-Directed, Post-Treatment Surveillance Colonoscopy in Early- and Late-Onset Colorectal Cancer Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Washington, Seattle, WA; 2Fred Hutchinson Cancer Center, Seattle, WA; 3Huntsman Cancer Institute, Salt Lake City, UT; 4University of Tennessee Health Science Center, Memphis, TN; 5Washington University School of Medicine in St. Louis, St. Louis, MO; 6Moffitt Cancer Center, Tampa, FL; 7Cedars-Sinai Medical Center, Los Angeles, CA; 8Heidelberg University Hospital, Heidelberg, Baden-Wurttemberg, Germany; 9University of Utah and Huntsman Cancer Institute, Salt Lake City, UT; 10UTHSC, Southaven, MS
Introduction: Recently, the incidence of early-onset colorectal cancer (eoCRC), diagnosed < 50 years old, has been rising. Current post-treatment surveillance guidelines for sporadic eoCRC and late-onset CRC (loCRC) recommend colonoscopies at intervals of 1- and 3-years (eg at 1- and 4-years after treatment). Given that eoCRC patients often present with advanced stage CRC, undergo more aggressive treatment and can have greater financial toxicity, we investigated if eoCRC patients’ compliance with recommended surveillance guidelines differs from loCRC patients.
Methods: We performed a retrospective cohort study of data from academic cancer centers, collected as part of a multicenter study following newly diagnosed CRC patients for 5 years. Demographics, dates of colonoscopies, cancer recurrence, and death were abstracted from medical records and patient questionnaires. Exclusion criteria were a diagnosis of Stage IV disease or undergoing total colectomy. Patients were followed until death, study withdrawal/completion, cancer recurrence, or date of most recent abstraction (8/31/23). The primary outcomes were undergoing guideline-directed colonoscopy at (1) 1-year and at (2) 1- and 4-years. Secondary outcomes were rate of undergoing colonoscopy at non-standard intervals of < 1-, 2-, or 3-years and overall rate of colonoscopies. Univariate and multivariable testing (controlling for stage, sex, BMI, smoking status, income, and education) was performed.
Results: Of 741 patients identified, 486 met inclusion criteria - of which 126 (26%) were eoCRC (Table). A total of 386/486 (79%) patients had ≥2 years of follow-up, of which 58/98 (60%) eoCRC and 152/288 (53%) loCRC patients underwent a colonoscopy at 1-year (OR 1.42,95% CI 0.86-2.37,p=0.17). A total of 263/486 (54%) patients had 5-years of follow-up, of which 15/65 (23%) eoCRC and 46/198 (23%) loCRC patients underwent a colonoscopy at 1-year and 4-years (OR 0.99,95% CI 0.51-1.93,p=0.98). Of all 486 patients, 64 (51%) eoCRC and 166 (46%) loCRC patients were screened at non-standard intervals (p=0.36). The rate of colonoscopies among all patients was 0.56/year, was 0.67 for eoCRC and 0.52 for loCRC (p=0.11).
Discussion: At the 1-year timepoint, eoCRC patients had a numerically higher rate of adherence to guideline-directed surveillance colonoscopy as compared to loCRC, but the magnitude of this difference was not large enough to be definitive. Both groups showed suboptimal compliance with post CRC surveillance guidelines in the 5 years following treatment.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Pakdee Rojanasopondist indicated no relevant financial relationships.
Ted Gooley indicated no relevant financial relationships.
Cornelia Ulrich indicated no relevant financial relationships.
Christopher Li indicated no relevant financial relationships.
David Shibata indicated no relevant financial relationships.
Adetunji Toriola indicated no relevant financial relationships.
Doratha Byrd indicated no relevant financial relationships.
Jane Figueiredo indicated no relevant financial relationships.
Biljana Gigic indicated no relevant financial relationships.
Sheetal Hardikar indicated no relevant financial relationships.
Stacey Cohen: Abbvie – Advisor or Review Panel Member. Agenus – Advisor or Review Panel Member. Biomea – Grant/Research Support. BNT – Grant/Research Support. Eisai – Advisor or Review Panel Member. Guardant – Advisor or Review Panel Member. Merck – Advisor or Review Panel Member. Pfizer – Consultant, Grant/Research Support. Regeneron – Advisor or Review Panel Member. Taiho – Advisor or Review Panel Member. Tempus – Grant/Research Support.
Lyen Huang indicated no relevant financial relationships.
Victoria Damerell indicated no relevant financial relationships.
Meghana Karchi indicated no relevant financial relationships.
Elizabeth Wood indicated no relevant financial relationships.
Ildiko Strehli indicated no relevant financial relationships.
William Grady: Diacarta – Consultant. GLG – Consultant. Guardant Health – Advisory Committee/Board Member. Guidepoint – Consultant. Karius – Consultant. UpToDate – Royalties.
Pakdee Rojanasopondist, MD1, Ted Gooley, PhD2, Cornelia Ulrich, PhD, MS3, Christopher I. Li, MD, PhD2, David Shibata, MD4, Adetunji Toriola, MD, PhD5, Doratha Byrd, PhD, MPH6, Jane C. Figueiredo, PhD7, Biljana Gigic, PhD, MSc8, Sheetal Hardikar, MBBS, PhD, MPH3, Stacey Cohen, MD2, Lyen Huang, MD, MPH9, Victoria Damerell, PhD8, Meghana V. Karchi, MPH10, Elizabeth H. Wood, MD4, Ildiko Strehli, PhD3, William M.. Grady, MD2. P3665 - Rates of Guideline-Directed, Post-Treatment Surveillance Colonoscopy in Early- and Late-Onset Colorectal Cancer Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

