Tuesday Poster Session
Category: Colon
P3666 - Variations in Aspirin, NSAIDs, Statins, and Metformin Use After Colorectal Cancer Treatment between Early- and Late-Onset Colorectal Cancer Patients in an International Multicenter Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Pakdee Rojanasopondist, MD
University of Washington
Seattle, WA
Presenting Author(s)
Pakdee Rojanasopondist, MD1, Ted Gooley, PhD2, Cornelia Ulrich, PhD, MS3, Christopher I. Li, MD, PhD2, David Shibata, MD4, Adetunji Toriola, MD, PhD5, Doratha Byrd, PhD, MPH6, Jane C. Figueiredo, PhD7, Biljana Gigic, PhD, MSc8, Sheetal Hardikar, MBBS, PhD, MPH3, Lyen Huang, MD, MPH9, Stacey Cohen, MD2, Victoria Damerell, PhD8, Meghana V. Karchi, MPH10, Elizabeth H. Wood, MD4, Ildiko Strehli, PhD3, William M.. Grady, MD2
1University of Washington, Seattle, WA; 2Fred Hutchinson Cancer Center, Seattle, WA; 3Huntsman Cancer Institute, Salt Lake City, UT; 4University of Tennessee Health Science Center, Memphis, TN; 5Washington University School of Medicine in St. Louis, St. Louis, MO; 6Moffitt Cancer Center, Tampa, FL; 7Cedars-Sinai Medical Center, Los Angeles, CA; 8Heidelberg University Hospital, Heidelberg, Baden-Wurttemberg, Germany; 9University of Utah and Huntsman Cancer Institute, Salt Lake City, UT; 10UTHSC, Southaven, MS
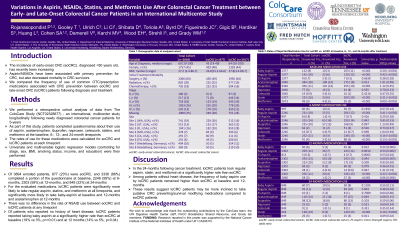
Introduction: The incidence of early-onset CRC (eoCRC), diagnosed < 50 years old, has recently been increasing. eoCRC patients face unique challenges after diagnosis and treatment that may shape their use of prescription or over-the-counter (OTC) medications. OTC medications may impact survivorship. For example, aspirin/NSAIDs have been associated with primary prevention for CRC, but also decreased mortality in CRC survivors. We compared the frequency of use of common OTC/prescription medications associated with CRC prevention between eoCRC and late-onset CRC (loCRC) patients following diagnosis and treatment.
Methods: We performed a retrospective cohort analysis of data from an international, multicenter study longitudinally following newly diagnosed colorectal cancer patients for 5-years. As part of this study, patients completed questionnaires about their use of aspirin, acetaminophen, ibuprofen, naproxen, celecoxib, statins, and metformin at the baseline, 6-, 12-, and 24-month timepoints. The rates of use for these medications were calculated for eoCRC and loCRC patients. Univariate and multivariable logistic regression models (controlling for stage, sex, BMI, smoking status, income, and education) were then performed.
Results: Of 3894 enrolled patients, 877 (23%) were eoCRC and 3336 (86%) completed a portion of the questionnaire at baseline, 2246 (58%) at 6-months, 2303 (59%) at 12-months, and 849 (22%) at 24-months (Table). For the evaluated medications, loCRC patients were significantly more likely to take regular aspirin, statins, and metformin at all timepoints, and significantly more likely to take baby-aspirin at baseline and 12-months and acetaminophen at 12-months. There was no difference in the rate of NSAID use between eoCRC and loCRC patients at any timepoint. Of patients who reported no history of heart disease, loCRC patients reported taking baby aspirin at a significantly higher rate than eoCRC at baseline (19% vs 3%, p=< 0.01) and at 12 months (14% vs 5%, p=0.04).
Discussion: In the 24-months following cancer treatment, loCRC patients took regular aspirin, statin, and metformin at a significantly higher rate than eoCRC. Among patients without heart disease, the frequency of baby aspirin use by loCRC patients remained higher than eoCRC at baseline and 12-months. These results suggest loCRC patients may be more inclined to take putative CRC preventing/survival modifying medications compared to eoCRC patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Pakdee Rojanasopondist, MD1, Ted Gooley, PhD2, Cornelia Ulrich, PhD, MS3, Christopher I. Li, MD, PhD2, David Shibata, MD4, Adetunji Toriola, MD, PhD5, Doratha Byrd, PhD, MPH6, Jane C. Figueiredo, PhD7, Biljana Gigic, PhD, MSc8, Sheetal Hardikar, MBBS, PhD, MPH3, Lyen Huang, MD, MPH9, Stacey Cohen, MD2, Victoria Damerell, PhD8, Meghana V. Karchi, MPH10, Elizabeth H. Wood, MD4, Ildiko Strehli, PhD3, William M.. Grady, MD2. P3666 - Variations in Aspirin, NSAIDs, Statins, and Metformin Use After Colorectal Cancer Treatment between Early- and Late-Onset Colorectal Cancer Patients in an International Multicenter Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Washington, Seattle, WA; 2Fred Hutchinson Cancer Center, Seattle, WA; 3Huntsman Cancer Institute, Salt Lake City, UT; 4University of Tennessee Health Science Center, Memphis, TN; 5Washington University School of Medicine in St. Louis, St. Louis, MO; 6Moffitt Cancer Center, Tampa, FL; 7Cedars-Sinai Medical Center, Los Angeles, CA; 8Heidelberg University Hospital, Heidelberg, Baden-Wurttemberg, Germany; 9University of Utah and Huntsman Cancer Institute, Salt Lake City, UT; 10UTHSC, Southaven, MS
Introduction: The incidence of early-onset CRC (eoCRC), diagnosed < 50 years old, has recently been increasing. eoCRC patients face unique challenges after diagnosis and treatment that may shape their use of prescription or over-the-counter (OTC) medications. OTC medications may impact survivorship. For example, aspirin/NSAIDs have been associated with primary prevention for CRC, but also decreased mortality in CRC survivors. We compared the frequency of use of common OTC/prescription medications associated with CRC prevention between eoCRC and late-onset CRC (loCRC) patients following diagnosis and treatment.
Methods: We performed a retrospective cohort analysis of data from an international, multicenter study longitudinally following newly diagnosed colorectal cancer patients for 5-years. As part of this study, patients completed questionnaires about their use of aspirin, acetaminophen, ibuprofen, naproxen, celecoxib, statins, and metformin at the baseline, 6-, 12-, and 24-month timepoints. The rates of use for these medications were calculated for eoCRC and loCRC patients. Univariate and multivariable logistic regression models (controlling for stage, sex, BMI, smoking status, income, and education) were then performed.
Results: Of 3894 enrolled patients, 877 (23%) were eoCRC and 3336 (86%) completed a portion of the questionnaire at baseline, 2246 (58%) at 6-months, 2303 (59%) at 12-months, and 849 (22%) at 24-months (Table). For the evaluated medications, loCRC patients were significantly more likely to take regular aspirin, statins, and metformin at all timepoints, and significantly more likely to take baby-aspirin at baseline and 12-months and acetaminophen at 12-months. There was no difference in the rate of NSAID use between eoCRC and loCRC patients at any timepoint. Of patients who reported no history of heart disease, loCRC patients reported taking baby aspirin at a significantly higher rate than eoCRC at baseline (19% vs 3%, p=< 0.01) and at 12 months (14% vs 5%, p=0.04).
Discussion: In the 24-months following cancer treatment, loCRC patients took regular aspirin, statin, and metformin at a significantly higher rate than eoCRC. Among patients without heart disease, the frequency of baby aspirin use by loCRC patients remained higher than eoCRC at baseline and 12-months. These results suggest loCRC patients may be more inclined to take putative CRC preventing/survival modifying medications compared to eoCRC patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Pakdee Rojanasopondist indicated no relevant financial relationships.
Ted Gooley indicated no relevant financial relationships.
Cornelia Ulrich indicated no relevant financial relationships.
Christopher Li indicated no relevant financial relationships.
David Shibata indicated no relevant financial relationships.
Adetunji Toriola indicated no relevant financial relationships.
Doratha Byrd indicated no relevant financial relationships.
Jane Figueiredo indicated no relevant financial relationships.
Biljana Gigic indicated no relevant financial relationships.
Sheetal Hardikar indicated no relevant financial relationships.
Lyen Huang indicated no relevant financial relationships.
Stacey Cohen: Abbvie – Advisor or Review Panel Member. Agenus – Advisor or Review Panel Member. Biomea – Grant/Research Support. BNT – Grant/Research Support. Eisai – Advisor or Review Panel Member. Guardant – Advisor or Review Panel Member. Merck – Advisor or Review Panel Member. Pfizer – Consultant, Grant/Research Support. Regeneron – Advisor or Review Panel Member. Taiho – Advisor or Review Panel Member. Tempus – Grant/Research Support.
Victoria Damerell indicated no relevant financial relationships.
Meghana Karchi indicated no relevant financial relationships.
Elizabeth Wood indicated no relevant financial relationships.
Ildiko Strehli indicated no relevant financial relationships.
William Grady: Diacarta – Consultant. GLG – Consultant. Guardant Health – Advisory Committee/Board Member. Guidepoint – Consultant. Karius – Consultant. UpToDate – Royalties.
Pakdee Rojanasopondist, MD1, Ted Gooley, PhD2, Cornelia Ulrich, PhD, MS3, Christopher I. Li, MD, PhD2, David Shibata, MD4, Adetunji Toriola, MD, PhD5, Doratha Byrd, PhD, MPH6, Jane C. Figueiredo, PhD7, Biljana Gigic, PhD, MSc8, Sheetal Hardikar, MBBS, PhD, MPH3, Lyen Huang, MD, MPH9, Stacey Cohen, MD2, Victoria Damerell, PhD8, Meghana V. Karchi, MPH10, Elizabeth H. Wood, MD4, Ildiko Strehli, PhD3, William M.. Grady, MD2. P3666 - Variations in Aspirin, NSAIDs, Statins, and Metformin Use After Colorectal Cancer Treatment between Early- and Late-Onset Colorectal Cancer Patients in an International Multicenter Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
