Tuesday Poster Session
Category: Colon
P3679 - A Rare Intersection: Pseudomembranous and Collagenous Colitis Mimicking Inflammatory Bowel Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Hiba Khan, MD
Virginia Commonwealth University Health System
Lake Grove, NY
Presenting Author(s)
Hiba Khan, MD1, Mahum Nadeem, MBBS2, Samia Liaquat, MD3, Milan Patel, MD4
1Virginia Commonwealth University Health System, Lake Grove, NY; 2Virginia Commonwealth University Health System, Henrico, VA; 3Virginia Commonwealth University Health System, Richmond, VA; 4Virginia Commonwealth University, Richmond, VA
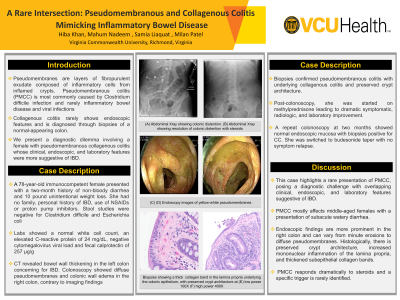
Introduction: Pseudomembranes are layers of fibropurulent exudate composed of inflammatory cells from inflamed crypts. This results in endothelial damage to the mucosa. Pseudomembranous colitis (PMC) is an inflammation of the colonic mucosa forming a yellow-white membrane, most commonly caused by Clostridium difficile infection. In rare cases, inflammatory bowel disease (IBD) and viral infections can also present as PMC. Collagenous colitis (CC) rarely shows endoscopic features and is diagnosed through biopsies of a normal-appearing colon. We present a diagnostic dilemma involving a female with pseudomembranous collagenous colitis (PMCC) whose clinical, endoscopic, and laboratory features were more suggestive of IBD.
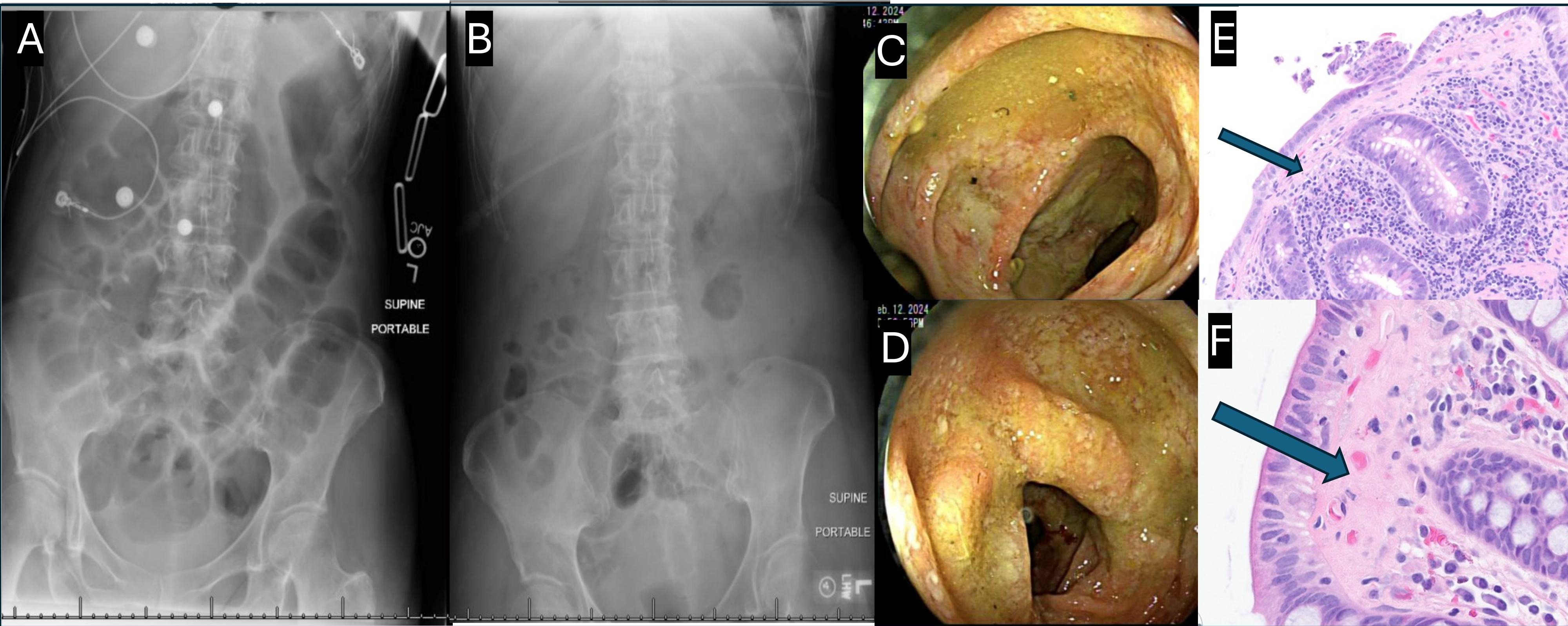
Case Description/Methods: A 78-year-old immunocompetent female presented with a two-month history of non-bloody diarrhea. She also reported a 10 pound unintentional weight loss. She had no family or personal history of IBD, or use of NSAIDs or proton pump inhibitors. Stool studies were negative for Clostridium difficile and Escherichia coli. Labs showed a normal white cell count, an elevated C-reactive protein (CRP) of 24 mg/dL, negative cytomegalovirus viral load and fecal calprotectin of 257 µg/g. Computerized Tomography (CT) imaging revealed bowel wall thickening in the left colon concerning for IBD. Colonoscopy showed diffuse pseudomembranes and colonic wall edema in the right colon, contrary to imaging findings. Biopsies confirmed pseudomembranous colitis with underlying collagenous colitis and preserved crypt architecture. Post-colonoscopy, she was started on methylprednisone leading to dramatic symptomatic, radiologic, and laboratory (CRP decreased from 24 to 2 mg/dL in two days) improvement. A repeat colonoscopy at two months showed normal endoscopic mucosa with biopsies positive for CC. She was switched to budesonide taper with no symptom relapse.
Discussion: This case highlights a rare presentation of PMCC, posing a diagnostic challenge with overlapping clinical, endoscopic, and laboratory features suggestive of IBD. PMCC more frequently affects middle-aged females with a presentation of subacute watery diarrhea. Endoscopic findings are more prominent in the right colon and can vary from minute erosions to diffuse pseudomembranes. Histologically, there is preserved crypt architecture, increased mononuclear inflammation of the lamina propria, and thickened subepithelial collagen bands. The condition responds dramatically to steroids and a specific trigger is rarely identified.
Disclosures:
Hiba Khan, MD1, Mahum Nadeem, MBBS2, Samia Liaquat, MD3, Milan Patel, MD4. P3679 - A Rare Intersection: Pseudomembranous and Collagenous Colitis Mimicking Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Virginia Commonwealth University Health System, Lake Grove, NY; 2Virginia Commonwealth University Health System, Henrico, VA; 3Virginia Commonwealth University Health System, Richmond, VA; 4Virginia Commonwealth University, Richmond, VA
Introduction: Pseudomembranes are layers of fibropurulent exudate composed of inflammatory cells from inflamed crypts. This results in endothelial damage to the mucosa. Pseudomembranous colitis (PMC) is an inflammation of the colonic mucosa forming a yellow-white membrane, most commonly caused by Clostridium difficile infection. In rare cases, inflammatory bowel disease (IBD) and viral infections can also present as PMC. Collagenous colitis (CC) rarely shows endoscopic features and is diagnosed through biopsies of a normal-appearing colon. We present a diagnostic dilemma involving a female with pseudomembranous collagenous colitis (PMCC) whose clinical, endoscopic, and laboratory features were more suggestive of IBD.
Case Description/Methods: A 78-year-old immunocompetent female presented with a two-month history of non-bloody diarrhea. She also reported a 10 pound unintentional weight loss. She had no family or personal history of IBD, or use of NSAIDs or proton pump inhibitors. Stool studies were negative for Clostridium difficile and Escherichia coli. Labs showed a normal white cell count, an elevated C-reactive protein (CRP) of 24 mg/dL, negative cytomegalovirus viral load and fecal calprotectin of 257 µg/g. Computerized Tomography (CT) imaging revealed bowel wall thickening in the left colon concerning for IBD. Colonoscopy showed diffuse pseudomembranes and colonic wall edema in the right colon, contrary to imaging findings. Biopsies confirmed pseudomembranous colitis with underlying collagenous colitis and preserved crypt architecture. Post-colonoscopy, she was started on methylprednisone leading to dramatic symptomatic, radiologic, and laboratory (CRP decreased from 24 to 2 mg/dL in two days) improvement. A repeat colonoscopy at two months showed normal endoscopic mucosa with biopsies positive for CC. She was switched to budesonide taper with no symptom relapse.
Discussion: This case highlights a rare presentation of PMCC, posing a diagnostic challenge with overlapping clinical, endoscopic, and laboratory features suggestive of IBD. PMCC more frequently affects middle-aged females with a presentation of subacute watery diarrhea. Endoscopic findings are more prominent in the right colon and can vary from minute erosions to diffuse pseudomembranes. Histologically, there is preserved crypt architecture, increased mononuclear inflammation of the lamina propria, and thickened subepithelial collagen bands. The condition responds dramatically to steroids and a specific trigger is rarely identified.
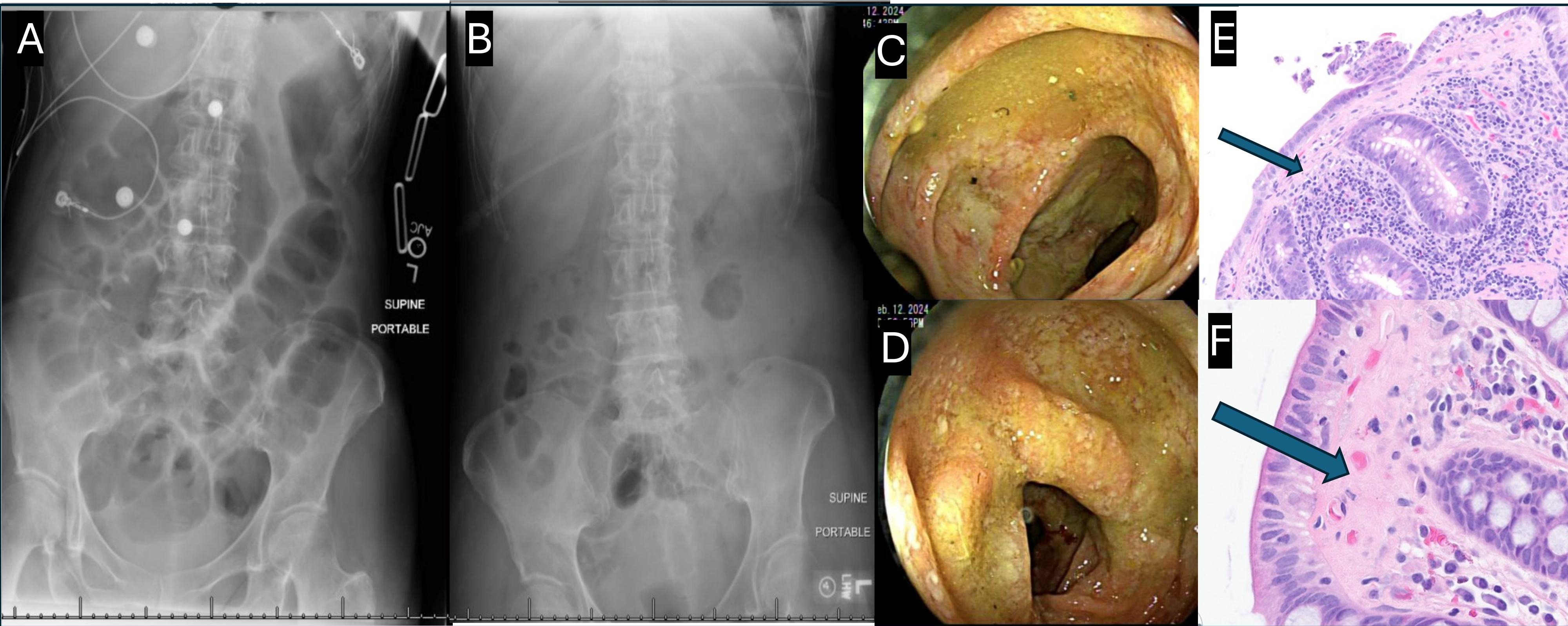
Figure: (A) Abdominal Xray showing colonic distention.
(B) Abdominal Xray showing resolution of colonic distention with steroids.
(C) (D) Endoscopy images of yellow-white pseudomembrane.
(E) (F) Right colon biopsy with arrows showing a marked collagen band in the lamina propria underlying the colonic epithelium, with preserved crypt architecture at (E) low power (hematoxylin-eosin [H&E],100X) and (F) high power view (H&E, 400X).
(B) Abdominal Xray showing resolution of colonic distention with steroids.
(C) (D) Endoscopy images of yellow-white pseudomembrane.
(E) (F) Right colon biopsy with arrows showing a marked collagen band in the lamina propria underlying the colonic epithelium, with preserved crypt architecture at (E) low power (hematoxylin-eosin [H&E],100X) and (F) high power view (H&E, 400X).
Disclosures:
Hiba Khan indicated no relevant financial relationships.
Mahum Nadeem indicated no relevant financial relationships.
Samia Liaquat indicated no relevant financial relationships.
Milan Patel indicated no relevant financial relationships.
Hiba Khan, MD1, Mahum Nadeem, MBBS2, Samia Liaquat, MD3, Milan Patel, MD4. P3679 - A Rare Intersection: Pseudomembranous and Collagenous Colitis Mimicking Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

