Tuesday Poster Session
Category: Colon
P3680 - Beyond the Surface: Navigating a Rare Colonic Anomaly - Mucosal Schwann Cell Hamartoma
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Dr. Valentina Saracino, DO
UNC Health Southeastern
Lumberton, NC
Presenting Author(s)
Dr. Valentina Saracino, DO, Dr. Rehman Chaudhry, DO, Dr. Kwadwo Agyei-Gyamfi, MD
UNC Health Southeastern, Lumberton, NC
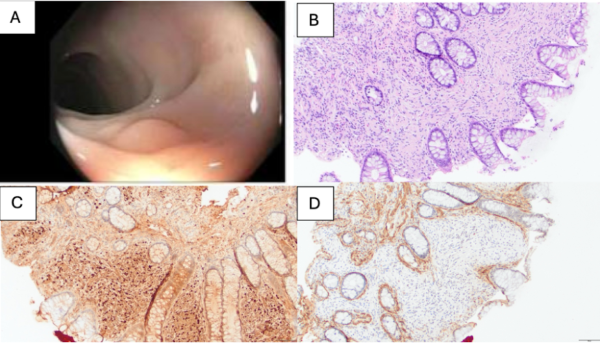
Introduction: A mucosal schwann cell hamartoma (MSCH) is a benign mucosal proliferation that is very rare and often found in the stomach rather than the colon or rectum. Diagnosis is primarily based on histological features, immunohistochemical pattern, and negative family history of NF1, MEN2, neural lesions or other syndromes. MSCH are often found incidentally, primarily through screening colonoscopies without any symptoms. An endoscopic evaluation is essential to rule out the presence of an underlying submucosal nodule or mass to assist with diagnosis.
Immunohistochemical patterns for MSCH include strong staining for S-100 protein in most cells as well as occasional positive staining for neurofilament protein (NFP) highlighted rare axons. MSCH are often confused with other pathologies including neurofibromas, gastrointestinal stromal tumors, mucosal neuromas, ganglioneuromas, and mucosal schwannomas, which lead to further aggressive therapy due to increased risk to transform into malignancy.
Case Description/Methods: A 53-year-old female with a past medical history of hypertension, GERD, non-insulin dependent type 2 diabetes mellitus, and endometrial uterine cancer who initially presented for screening colonoscopy. She denied having any current complaints including diarrhea, constipation, or blood in the stool. She had no family history of colon cancer and no history of familial adenomatous polyposis.
She then received a colonoscopy that was remarkable for a 5 mm colon polyp within the distal descending colon. Pathology showed bland spindle cell proliferation within the lamina propria and cells that were strongly positive for S100, but negative for smooth muscle actin, consistent with a mucosal Schwann cell hamartoma.
Discussion: MSCH are uncommon benign colon findings that are clinically important to diagnose to prevent unnecessary aggressive therapy. Diagnosis relies on histological features, immunohistochemical pattern, and the absence of a family history of NF1, MEN2, neural lesions, or other syndromes. MSCH can mimic many other conditions that have increased malignancy potential including those associated with inherited syndromes such as NF1, MEN2B, and Cowden [5].
For example, neurofibromas and MSCHs can both appear as spindle cell lesions in the gastrointestinal tract, however, MSCHs tend to have virtually all cells stain positive for S-100. Gastrointestinal stromal tumors are also similar, but have positive CD117 immunohistochemical staining and the presence of ganglion cells.
Disclosures:
Dr. Valentina Saracino, DO, Dr. Rehman Chaudhry, DO, Dr. Kwadwo Agyei-Gyamfi, MD. P3680 - Beyond the Surface: Navigating a Rare Colonic Anomaly - Mucosal Schwann Cell Hamartoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
UNC Health Southeastern, Lumberton, NC
Introduction: A mucosal schwann cell hamartoma (MSCH) is a benign mucosal proliferation that is very rare and often found in the stomach rather than the colon or rectum. Diagnosis is primarily based on histological features, immunohistochemical pattern, and negative family history of NF1, MEN2, neural lesions or other syndromes. MSCH are often found incidentally, primarily through screening colonoscopies without any symptoms. An endoscopic evaluation is essential to rule out the presence of an underlying submucosal nodule or mass to assist with diagnosis.
Immunohistochemical patterns for MSCH include strong staining for S-100 protein in most cells as well as occasional positive staining for neurofilament protein (NFP) highlighted rare axons. MSCH are often confused with other pathologies including neurofibromas, gastrointestinal stromal tumors, mucosal neuromas, ganglioneuromas, and mucosal schwannomas, which lead to further aggressive therapy due to increased risk to transform into malignancy.
Case Description/Methods: A 53-year-old female with a past medical history of hypertension, GERD, non-insulin dependent type 2 diabetes mellitus, and endometrial uterine cancer who initially presented for screening colonoscopy. She denied having any current complaints including diarrhea, constipation, or blood in the stool. She had no family history of colon cancer and no history of familial adenomatous polyposis.
She then received a colonoscopy that was remarkable for a 5 mm colon polyp within the distal descending colon. Pathology showed bland spindle cell proliferation within the lamina propria and cells that were strongly positive for S100, but negative for smooth muscle actin, consistent with a mucosal Schwann cell hamartoma.
Discussion: MSCH are uncommon benign colon findings that are clinically important to diagnose to prevent unnecessary aggressive therapy. Diagnosis relies on histological features, immunohistochemical pattern, and the absence of a family history of NF1, MEN2, neural lesions, or other syndromes. MSCH can mimic many other conditions that have increased malignancy potential including those associated with inherited syndromes such as NF1, MEN2B, and Cowden [5].
For example, neurofibromas and MSCHs can both appear as spindle cell lesions in the gastrointestinal tract, however, MSCHs tend to have virtually all cells stain positive for S-100. Gastrointestinal stromal tumors are also similar, but have positive CD117 immunohistochemical staining and the presence of ganglion cells.
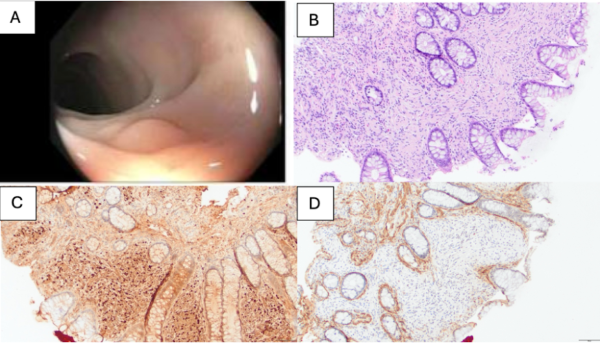
Figure: Image A: Colonoscopy showing sessile descending colon polyp approximately 5 mm in size.
Image B: H&E staining of colon polyp with simple columnar epithelium, numerous goblet cells, and intestinal glands.
Image C: S100 positive immunohistochemical staining critical for identifying a schwannoma.
Image D: Negative smooth muscle actin staining.
Image B: H&E staining of colon polyp with simple columnar epithelium, numerous goblet cells, and intestinal glands.
Image C: S100 positive immunohistochemical staining critical for identifying a schwannoma.
Image D: Negative smooth muscle actin staining.
Disclosures:
Dr. Valentina Saracino indicated no relevant financial relationships.
Dr. Rehman Chaudhry indicated no relevant financial relationships.
Dr. Kwadwo Agyei-Gyamfi indicated no relevant financial relationships.
Dr. Valentina Saracino, DO, Dr. Rehman Chaudhry, DO, Dr. Kwadwo Agyei-Gyamfi, MD. P3680 - Beyond the Surface: Navigating a Rare Colonic Anomaly - Mucosal Schwann Cell Hamartoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
