Tuesday Poster Session
Category: Biliary/Pancreas
P3583 - Unmasking the Hidden Foe: Signet Ring Cell Carcinoma of the Ampulla of Vater Discovered Post-Cholecystectomy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Cristoffer Rivera, MD
HCA Florida Healthcare
Miami, FL
Presenting Author(s)
Cristoffer Rivera, MD1, Jose Melendez, MD1, Jose Gonzalez, MD1, Jorge Suarez, MD2, Khitani Amit, MD1
1HCA Florida Healthcare, Miami, FL; 2HCA Florida Kendall Hospital, Miami, FL
Introduction: Carcinoma of the ampulla of Vater accounts for 0.2% of all gastrointestinal malignancies and less than 6% of all periampullary cancers but is responsible for 20% of all tumor-related obstructions of the common bile duct. It has no racial or ethnic predisposition and no gender preference. As per the World Journal of Gastroenterology, age-specific incidence rates are slightly higher in men than in women. The incidence of ampullary tumors is increased 200 to 300-fold among patients with hereditary polyposis syndromes, such as familial adenomatous polyposis and hereditary nonpolyposis colorectal cancer, compared with the general population.
Case Description/Methods: Here we present a case of a 62-year-old male with no significant past medical history who presented complaining of pruritus and jaundice for the past 4 days. One month before the presenting symptoms the patient underwent Robotic robotic-assisted cholecystectomy after presenting with post-prandial pain associated with PO intolerance.
Upon arrival at our institution, the patient was hemodynamically stable, and laboratory results were significant for elevated Total Bilirubin, Hepatic enzymes, and Lipase. Imaging studies such as MRCP showed focal irregular thickening of the duodenum at the level of the ampulla measuring approximately 2.7 x 3.7 x 1.9 cm. A Pancreas Protocol CT Scan abdomen/pelvis was done afterward with findings significant for a 3.3 x 1.7 x 2.4 cm periampullary mass with close association to the duodenum rather than the pancreas with a protruding component into the common bile duct. Chest CT Scan was also done with no metastatic disease findings reported.
Followed by ERCP with results consistent with duodenal bulb mass. Biopsy was obtained
After a thorough review of imaging results in conjunction with the Oncology Surgery Service and with patient consent decision was made to pursue Whipple Procedure with feeding jejunostomy tube placement.
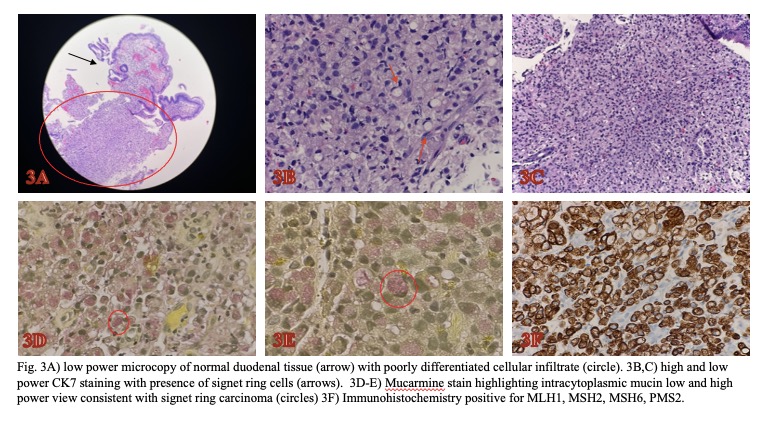
Pathology results of the duodenal mass biopsy were significant for poorly differentiated adenocarcinoma with signet ring cell features. Immunohistochemistry positive for MLH1, MSH2, MSH6, PMS2.
Discussion: This case report illustrates the critical need for vigilance in the diagnosis of persistent post-cholecystectomy symptoms. SRCA of the Ampulla of Vater, although rare, should be considered in the differential diagnosis. A Multidisciplinary approach is essential for timely diagnosis and management as this improves the patient's prognosis with such rare and aggressive malignancy.
Disclosures:
Cristoffer Rivera, MD1, Jose Melendez, MD1, Jose Gonzalez, MD1, Jorge Suarez, MD2, Khitani Amit, MD1. P3583 - Unmasking the Hidden Foe: Signet Ring Cell Carcinoma of the Ampulla of Vater Discovered Post-Cholecystectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HCA Florida Healthcare, Miami, FL; 2HCA Florida Kendall Hospital, Miami, FL
Introduction: Carcinoma of the ampulla of Vater accounts for 0.2% of all gastrointestinal malignancies and less than 6% of all periampullary cancers but is responsible for 20% of all tumor-related obstructions of the common bile duct. It has no racial or ethnic predisposition and no gender preference. As per the World Journal of Gastroenterology, age-specific incidence rates are slightly higher in men than in women. The incidence of ampullary tumors is increased 200 to 300-fold among patients with hereditary polyposis syndromes, such as familial adenomatous polyposis and hereditary nonpolyposis colorectal cancer, compared with the general population.
Case Description/Methods: Here we present a case of a 62-year-old male with no significant past medical history who presented complaining of pruritus and jaundice for the past 4 days. One month before the presenting symptoms the patient underwent Robotic robotic-assisted cholecystectomy after presenting with post-prandial pain associated with PO intolerance.
Upon arrival at our institution, the patient was hemodynamically stable, and laboratory results were significant for elevated Total Bilirubin, Hepatic enzymes, and Lipase. Imaging studies such as MRCP showed focal irregular thickening of the duodenum at the level of the ampulla measuring approximately 2.7 x 3.7 x 1.9 cm. A Pancreas Protocol CT Scan abdomen/pelvis was done afterward with findings significant for a 3.3 x 1.7 x 2.4 cm periampullary mass with close association to the duodenum rather than the pancreas with a protruding component into the common bile duct. Chest CT Scan was also done with no metastatic disease findings reported.
Followed by ERCP with results consistent with duodenal bulb mass. Biopsy was obtained
After a thorough review of imaging results in conjunction with the Oncology Surgery Service and with patient consent decision was made to pursue Whipple Procedure with feeding jejunostomy tube placement.
Pathology results of the duodenal mass biopsy were significant for poorly differentiated adenocarcinoma with signet ring cell features. Immunohistochemistry positive for MLH1, MSH2, MSH6, PMS2.
Discussion: This case report illustrates the critical need for vigilance in the diagnosis of persistent post-cholecystectomy symptoms. SRCA of the Ampulla of Vater, although rare, should be considered in the differential diagnosis. A Multidisciplinary approach is essential for timely diagnosis and management as this improves the patient's prognosis with such rare and aggressive malignancy.
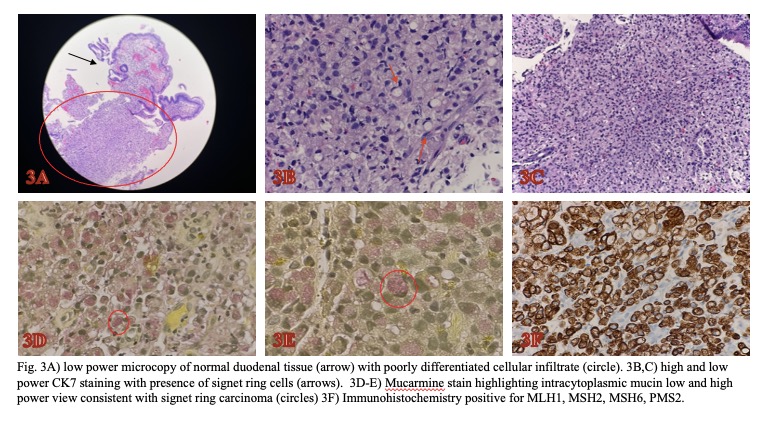
Figure: Immunohistochemistry
Disclosures:
Cristoffer Rivera indicated no relevant financial relationships.
Jose Melendez indicated no relevant financial relationships.
Jose Gonzalez indicated no relevant financial relationships.
Jorge Suarez indicated no relevant financial relationships.
Khitani Amit indicated no relevant financial relationships.
Cristoffer Rivera, MD1, Jose Melendez, MD1, Jose Gonzalez, MD1, Jorge Suarez, MD2, Khitani Amit, MD1. P3583 - Unmasking the Hidden Foe: Signet Ring Cell Carcinoma of the Ampulla of Vater Discovered Post-Cholecystectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

