Tuesday Poster Session
Category: Biliary/Pancreas
P3584 - Pancreatic Lymphoma: A Familiar Entity at an Unusual Location - A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Muhamad Oum, MD
Saint Agnes Medical Center
Fresno, CA
Presenting Author(s)
Muhamad Oum, MD1, Saif M.. Srouji, MD1, Celise Nardes Ferreira, MD1, Nicholas Reyes, MD1, Nathanael A. Reyes, MD2, Mehdi Hakimipour, MD1, Anupama Poliyedath, MD3
1Saint Agnes Medical Center, Fresno, CA; 2St. Agnes Medical Center, Fresno, CA; 3St. Agnes Internal Medicine Residency, Fresno, CA
Introduction: Primary pancreatic lymphoma (PPL) is a rare entity, comprising just 0.1%-1.5% of all pancreatic cancers, with diffuse large B-cell lymphoma (DLBCL) being its most frequent subtype, representing 77%-80% of cases. The clinical and imaging resemblance of PPL to other pancreatic malignancies poses significant diagnostic challenges. Nevertheless, distinguishing PPL is crucial because, in contrast to other pancreatic tumors, it is potentially curable with chemotherapy and radiotherapy, highlighting the importance of accurate diagnosis and management to optimize outcomes.
Case Description/Methods: A 59-year-old male with a history of successfully treated H. pylori-related peptic ulcer disease presented with persistent epigastric pain, fatigue, and an unintentional weight loss of 5 pounds over a month. Initial lab tests revealed a slightly elevated lipase level, but other parameters were within normal ranges. An abdominal ultrasound showed gallbladder sludge without signs of cholecystitis, and the pancreas appeared normal. Despite pantoprazole therapy, his symptoms persisted, necessitating further evaluation. Subsequent tests showed elevated lipase levels and mild normocytic anemia. Abdomen and pelvis contrast-enhanced CT scan revealed a suspicious mass encasing the superior mesenteric artery and adjacent enlarged mesenteric lymph nodes, raising concerns for primary pancreatic malignancy. A CT-guided biopsy confirmed the diagnosis of diffuse large B-cell lymphoma. Patient is currently being treated with R-CHOP chemotherapy.
Discussion: PPL, particularly DLBCL, poses a unique clinical challenge due to its rarity and nonspecific presentation, closely mimicking other pancreatic pathologies. This malignancy predominantly affects the elderly, with a slight male predominance, and can manifest symptoms common to other pancreatic diseases, such as abdominal pain, jaundice, and weight loss. The case emphasizes the critical role of comprehensive diagnostic strategies, including advanced imaging techniques and histopathological confirmation, in distinguishing PPL from more common pancreatic adenocarcinomas. Given the potential for curative treatment with chemotherapy, as demonstrated in this case where the patient is responding favorably to R-CHOP therapy, early and accurate diagnosis becomes paramount. This report highlights the importance of including PPL in the differential diagnosis of pancreatic masses, ensuring timely and appropriate therapeutic interventions that can significantly improve patient outcomes.

Disclosures:
Muhamad Oum, MD1, Saif M.. Srouji, MD1, Celise Nardes Ferreira, MD1, Nicholas Reyes, MD1, Nathanael A. Reyes, MD2, Mehdi Hakimipour, MD1, Anupama Poliyedath, MD3. P3584 - Pancreatic Lymphoma: A Familiar Entity at an Unusual Location - A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Agnes Medical Center, Fresno, CA; 2St. Agnes Medical Center, Fresno, CA; 3St. Agnes Internal Medicine Residency, Fresno, CA
Introduction: Primary pancreatic lymphoma (PPL) is a rare entity, comprising just 0.1%-1.5% of all pancreatic cancers, with diffuse large B-cell lymphoma (DLBCL) being its most frequent subtype, representing 77%-80% of cases. The clinical and imaging resemblance of PPL to other pancreatic malignancies poses significant diagnostic challenges. Nevertheless, distinguishing PPL is crucial because, in contrast to other pancreatic tumors, it is potentially curable with chemotherapy and radiotherapy, highlighting the importance of accurate diagnosis and management to optimize outcomes.
Case Description/Methods: A 59-year-old male with a history of successfully treated H. pylori-related peptic ulcer disease presented with persistent epigastric pain, fatigue, and an unintentional weight loss of 5 pounds over a month. Initial lab tests revealed a slightly elevated lipase level, but other parameters were within normal ranges. An abdominal ultrasound showed gallbladder sludge without signs of cholecystitis, and the pancreas appeared normal. Despite pantoprazole therapy, his symptoms persisted, necessitating further evaluation. Subsequent tests showed elevated lipase levels and mild normocytic anemia. Abdomen and pelvis contrast-enhanced CT scan revealed a suspicious mass encasing the superior mesenteric artery and adjacent enlarged mesenteric lymph nodes, raising concerns for primary pancreatic malignancy. A CT-guided biopsy confirmed the diagnosis of diffuse large B-cell lymphoma. Patient is currently being treated with R-CHOP chemotherapy.
Discussion: PPL, particularly DLBCL, poses a unique clinical challenge due to its rarity and nonspecific presentation, closely mimicking other pancreatic pathologies. This malignancy predominantly affects the elderly, with a slight male predominance, and can manifest symptoms common to other pancreatic diseases, such as abdominal pain, jaundice, and weight loss. The case emphasizes the critical role of comprehensive diagnostic strategies, including advanced imaging techniques and histopathological confirmation, in distinguishing PPL from more common pancreatic adenocarcinomas. Given the potential for curative treatment with chemotherapy, as demonstrated in this case where the patient is responding favorably to R-CHOP therapy, early and accurate diagnosis becomes paramount. This report highlights the importance of including PPL in the differential diagnosis of pancreatic masses, ensuring timely and appropriate therapeutic interventions that can significantly improve patient outcomes.

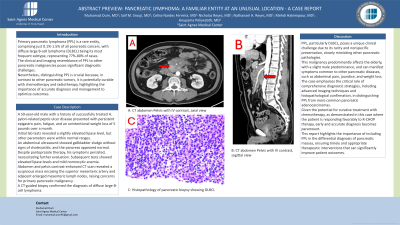
Figure: A: CT abdomen Pelvis with IV contrast, axial view.
B: CT abdomen Pelvis with IV contrast, sagittal view
C: Histopathology of pancreatic biopsy showing DLBCL
B: CT abdomen Pelvis with IV contrast, sagittal view
C: Histopathology of pancreatic biopsy showing DLBCL
Disclosures:
Muhamad Oum indicated no relevant financial relationships.
Saif Srouji indicated no relevant financial relationships.
Celise Nardes Ferreira indicated no relevant financial relationships.
Nicholas Reyes indicated no relevant financial relationships.
Nathanael Reyes indicated no relevant financial relationships.
Mehdi Hakimipour indicated no relevant financial relationships.
Anupama Poliyedath indicated no relevant financial relationships.
Muhamad Oum, MD1, Saif M.. Srouji, MD1, Celise Nardes Ferreira, MD1, Nicholas Reyes, MD1, Nathanael A. Reyes, MD2, Mehdi Hakimipour, MD1, Anupama Poliyedath, MD3. P3584 - Pancreatic Lymphoma: A Familiar Entity at an Unusual Location - A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
