Tuesday Poster Session
Category: Biliary/Pancreas
P3585 - To Re-Stent or Not to Re-Stent: A Rare Case of Recurrent Hemobilia From a Hepatic Artery Pseudoaneurysm
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Mena Saad, DO
Riverside University Health System
Moreno Valley, CA
Presenting Author(s)
Mena Saad, DO1, Jun Song, MD2, Harold J. Duarte, MD3, Emily Lin, MD2, Raul Hernandez, MD4, Christopher Bent, MD1, Wichit Srikureja, MD1, Manish Shrestha, MD1, Steve Serrao, MD1
1Riverside University Health System, Moreno Valley, CA; 2Loma Linda University Medical Center, Loma Linda, CA; 3Loma Linda University Health, Loma Linda, CA; 4Riverside University Health System, Redlands, CA
Introduction: Hemobilia resulting from pseudoaneurysm (PSA) dissection is uncommon, but potentially fatal. We present a case of recurrent hemobilia secondary to a hepatic artery pseudoaneurysm.
Case Description/Methods: A 52-year-old female with a history of cirrhosis presented with two days of generalized abdominal pain and vomiting. Initial laboratory studies were significant for elevated liver enzymes. Physical exam was notable for right upper quadrant tenderness, and vital signs were within normal limits. Imaging showed acute cholecystitis. During laparoscopic cholecystectomy, urgent endoscopic retrograde cholangiopancreatography (ERCP) was done to rule out bile duct injury as hemobilia was encountered intraoperatively. ERCP was completed with stone extraction and a self-expanding metal stent was placed in the CBD. Mucosal epinephrine was also administered to control sphincterotomy bleeding. Due to continued bleeding, CT abdomen and pelvis was ordered and demonstrated a hepatic artery PSA with thrombus to the mid/distal segment. Due to recurrent hemobilia, repeat ERCP was done with continued bleeding seen coming through the existing biliary stent leading to a second CBD stent being placed. A third ERCP was done to place a third biliary stent below the bifurcation of the left and right intrahepatic duct with resolution of the hemobilia. Due to an increase in the hepatic artery PSA, Interventional radiology (IR) completed a celiac arteriogram which demonstrated a pseudoaneurysm arising from the gastroduodenal artery near its origin from the proper hepatic artery. Successful coil embolization was completed with collateral flow to the liver arising from the gastroduodenal and left gastric arteries. The patient's liver enzymes improved and she experienced no further episodes of melena. Hemoglobin stabilized and the patient was safely discharged.
Discussion: Hemobilia is an uncommon cause of gastrointestinal bleeding and typically is a complication after invasive procedures that involve the liver, pancreas, biliary tree, and/or its vasculature. Recognizing vascular causes of hemobilia is critical and IR embolization should be considered early. Identifying the extent of collateral flow to the liver could potentially prevent acute decompensation and liver failure. Transfer to a center with liver transplant capabilities due to increased rates of acute liver failure following IR embolization is also an important consideration.
Disclosures:
Mena Saad, DO1, Jun Song, MD2, Harold J. Duarte, MD3, Emily Lin, MD2, Raul Hernandez, MD4, Christopher Bent, MD1, Wichit Srikureja, MD1, Manish Shrestha, MD1, Steve Serrao, MD1. P3585 - To Re-Stent or Not to Re-Stent: A Rare Case of Recurrent Hemobilia From a Hepatic Artery Pseudoaneurysm, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Riverside University Health System, Moreno Valley, CA; 2Loma Linda University Medical Center, Loma Linda, CA; 3Loma Linda University Health, Loma Linda, CA; 4Riverside University Health System, Redlands, CA
Introduction: Hemobilia resulting from pseudoaneurysm (PSA) dissection is uncommon, but potentially fatal. We present a case of recurrent hemobilia secondary to a hepatic artery pseudoaneurysm.
Case Description/Methods: A 52-year-old female with a history of cirrhosis presented with two days of generalized abdominal pain and vomiting. Initial laboratory studies were significant for elevated liver enzymes. Physical exam was notable for right upper quadrant tenderness, and vital signs were within normal limits. Imaging showed acute cholecystitis. During laparoscopic cholecystectomy, urgent endoscopic retrograde cholangiopancreatography (ERCP) was done to rule out bile duct injury as hemobilia was encountered intraoperatively. ERCP was completed with stone extraction and a self-expanding metal stent was placed in the CBD. Mucosal epinephrine was also administered to control sphincterotomy bleeding. Due to continued bleeding, CT abdomen and pelvis was ordered and demonstrated a hepatic artery PSA with thrombus to the mid/distal segment. Due to recurrent hemobilia, repeat ERCP was done with continued bleeding seen coming through the existing biliary stent leading to a second CBD stent being placed. A third ERCP was done to place a third biliary stent below the bifurcation of the left and right intrahepatic duct with resolution of the hemobilia. Due to an increase in the hepatic artery PSA, Interventional radiology (IR) completed a celiac arteriogram which demonstrated a pseudoaneurysm arising from the gastroduodenal artery near its origin from the proper hepatic artery. Successful coil embolization was completed with collateral flow to the liver arising from the gastroduodenal and left gastric arteries. The patient's liver enzymes improved and she experienced no further episodes of melena. Hemoglobin stabilized and the patient was safely discharged.
Discussion: Hemobilia is an uncommon cause of gastrointestinal bleeding and typically is a complication after invasive procedures that involve the liver, pancreas, biliary tree, and/or its vasculature. Recognizing vascular causes of hemobilia is critical and IR embolization should be considered early. Identifying the extent of collateral flow to the liver could potentially prevent acute decompensation and liver failure. Transfer to a center with liver transplant capabilities due to increased rates of acute liver failure following IR embolization is also an important consideration.
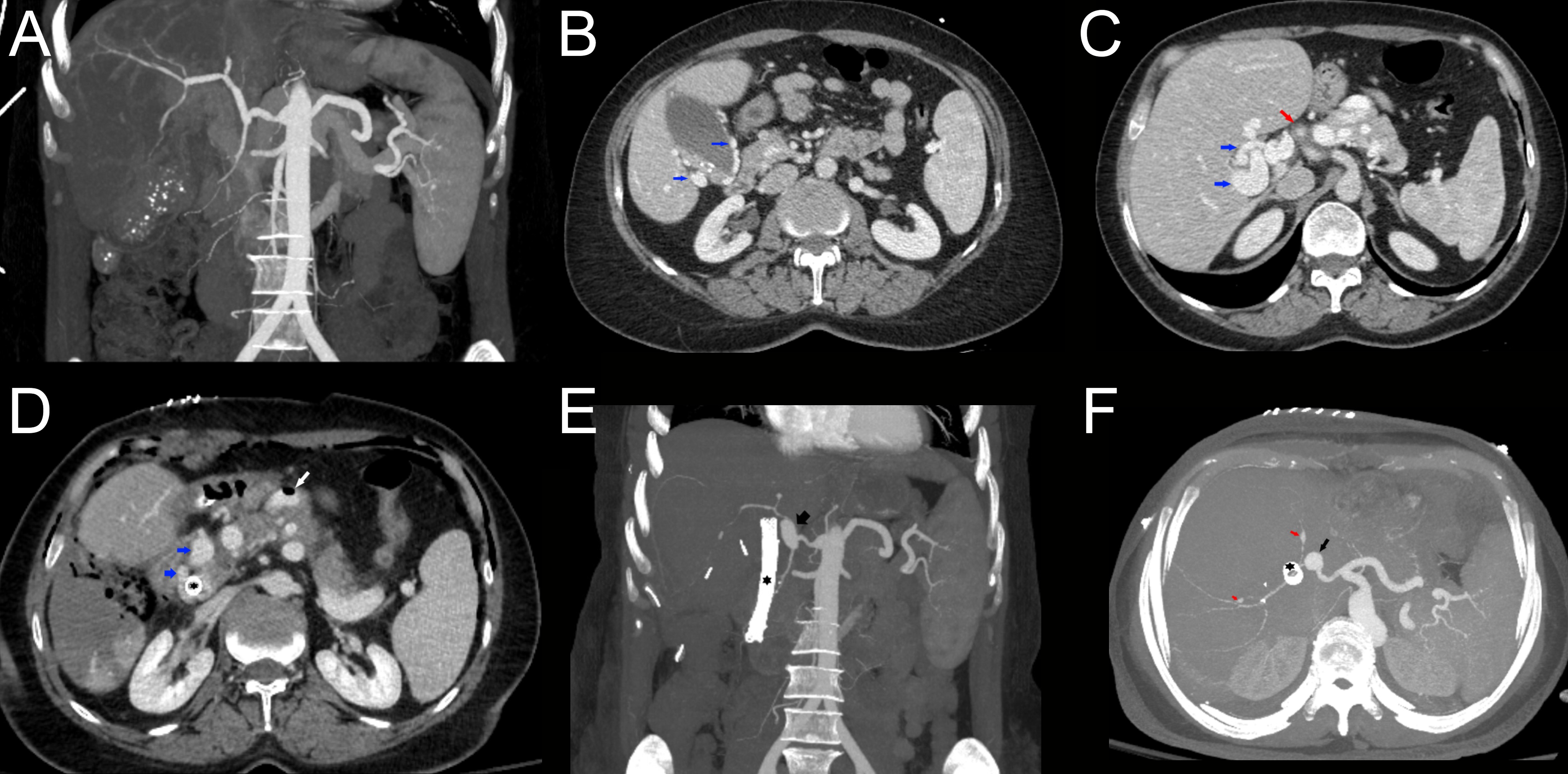
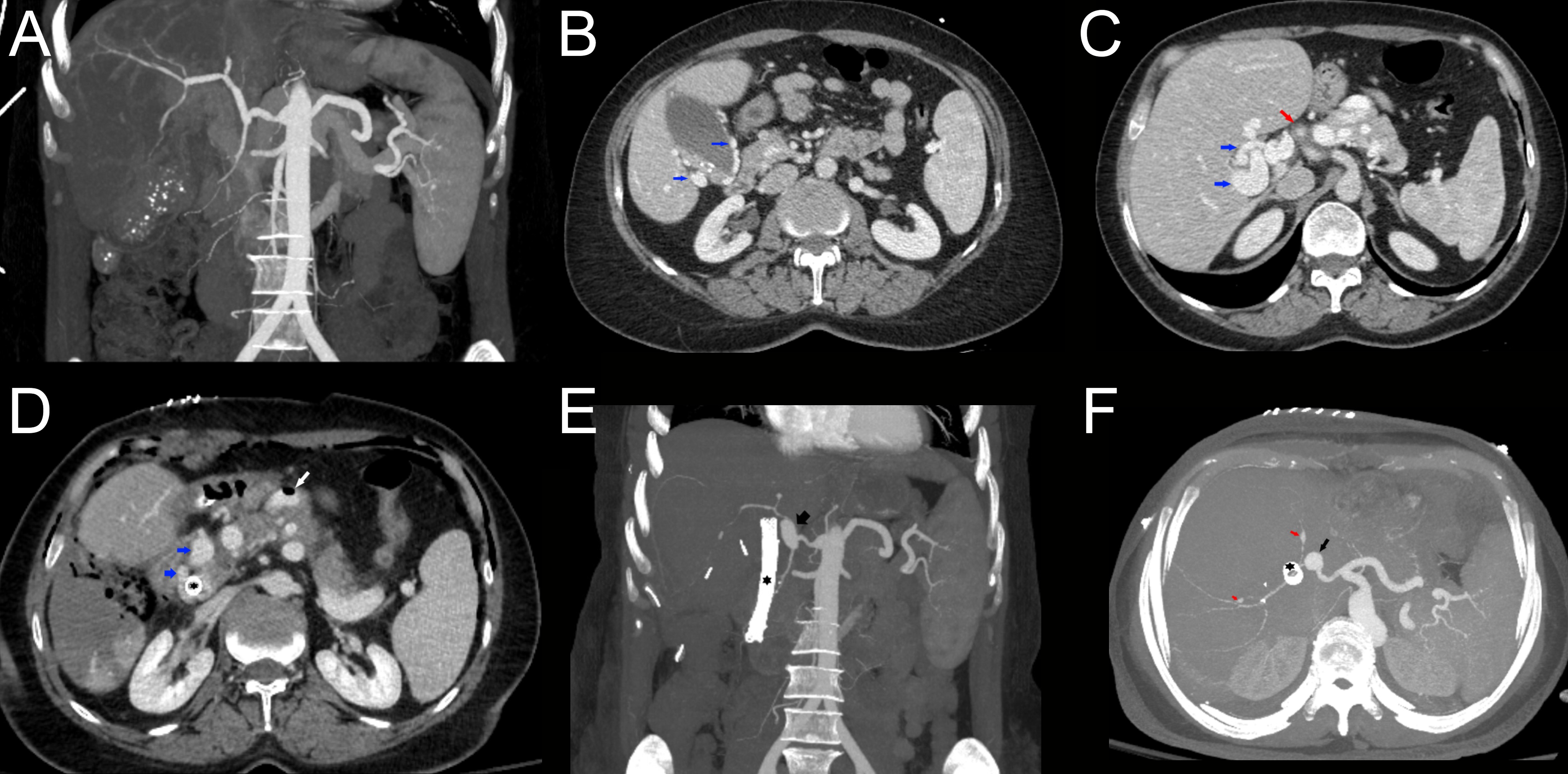
Figure: Figure A: CTA coronal max intensity pre-base line shows no aneurysm.
Figure B: CT axial post-contrast venous phase image shows: gallbladder with dilated varices in gallbladder wall (blue arrows).
Figure C: CT axial post-contrast venous phase image shows: portal venous varices/cavernous transformation of the portal vein consistent with chronic PV occlusion (blue arrows). Proper hepatic artery (red arrow) with normal caliber but thickened wall suggesting possible vasculitis.
Figure D: Postcholecystectomy and CBD stent procedure CT axial post-contrast venous phase image shows: CBD stent (black star) surrounded by dilated cavernous varices (blue arrow). Air is noted post-intervention in one of the dilated portomesenteric varices along the anterior pancreas (white arrow). Also, note postoperative pneumoperitoneum and air in the gallbladder fossa.
Figure E: Post cholecystectomy and CBD stent procedure CT coronal post-contrast arterial maximum intensity image shows: arterial pseudoaneurysm at the origin of proper hepatic and gastroduodenal arteries (black arrow). Note CBD stent (black star).
Figure F: Postcholecystectomy and CBD stent procedure CT axial post-contrast arterial maximum intensity image shows: arterial pseudoaneurysm at the origin of proper hepatic and gastroduodenal arteries (black arrow). Two small foci of arterial dilatation noted within the arterial branches of the liver (red arrows) suspicious for underlying vasculitis. Note CBD stent (black star).
Figure B: CT axial post-contrast venous phase image shows: gallbladder with dilated varices in gallbladder wall (blue arrows).
Figure C: CT axial post-contrast venous phase image shows: portal venous varices/cavernous transformation of the portal vein consistent with chronic PV occlusion (blue arrows). Proper hepatic artery (red arrow) with normal caliber but thickened wall suggesting possible vasculitis.
Figure D: Postcholecystectomy and CBD stent procedure CT axial post-contrast venous phase image shows: CBD stent (black star) surrounded by dilated cavernous varices (blue arrow). Air is noted post-intervention in one of the dilated portomesenteric varices along the anterior pancreas (white arrow). Also, note postoperative pneumoperitoneum and air in the gallbladder fossa.
Figure E: Post cholecystectomy and CBD stent procedure CT coronal post-contrast arterial maximum intensity image shows: arterial pseudoaneurysm at the origin of proper hepatic and gastroduodenal arteries (black arrow). Note CBD stent (black star).
Figure F: Postcholecystectomy and CBD stent procedure CT axial post-contrast arterial maximum intensity image shows: arterial pseudoaneurysm at the origin of proper hepatic and gastroduodenal arteries (black arrow). Two small foci of arterial dilatation noted within the arterial branches of the liver (red arrows) suspicious for underlying vasculitis. Note CBD stent (black star).
Disclosures:
Mena Saad indicated no relevant financial relationships.
Jun Song indicated no relevant financial relationships.
Harold Duarte indicated no relevant financial relationships.
Emily Lin indicated no relevant financial relationships.
Raul Hernandez indicated no relevant financial relationships.
Christopher Bent indicated no relevant financial relationships.
Wichit Srikureja indicated no relevant financial relationships.
Manish Shrestha indicated no relevant financial relationships.
Steve Serrao: Provation Medical – Advisory Committee/Board Member.
Mena Saad, DO1, Jun Song, MD2, Harold J. Duarte, MD3, Emily Lin, MD2, Raul Hernandez, MD4, Christopher Bent, MD1, Wichit Srikureja, MD1, Manish Shrestha, MD1, Steve Serrao, MD1. P3585 - To Re-Stent or Not to Re-Stent: A Rare Case of Recurrent Hemobilia From a Hepatic Artery Pseudoaneurysm, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
