Tuesday Poster Session
Category: Biliary/Pancreas
P3508 - From High to Harm: A Case of Cannabis-Induced Pancreatitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Walaa Hasan, MD
Trinitas Regional Medical Center
Cranford, NJ
Presenting Author(s)
Walaa Hasan, MD1, Aryeh Moskovits, DO2, Stephen Dimaggio, MD2, Farah Faridi, MD2
1Trinitas Regional Medical Center, Elizabeth, NJ; 2RWJ Barnabas Health, Trinitas Regional Medical Center, Elizabeth, NJ
Introduction: Cannabis consumption is increasing due to its legalization for medical and recreational use. While its effects on the central nervous system are well-known, its impact on other organ systems is less understood. This case report presents a rare instance of acute pancreatitis triggered by cannabis use.
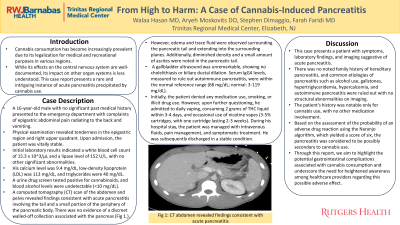
Case Description/Methods: A 16-year-old male with no significant medical history presented with epigastric abdominal pain radiating to the back and vomiting. Physical examination revealed tenderness in the epigastric region and right upper quadrant. The patient was vitally stable. Initial lab results showed a white blood cell count of 15.3 x 10^3/μL and a lipase level of 152 U/L. His calcium level was 9.4 mg/dL, LDL was 113 mg/dL, and triglycerides were 40 mg/dL. A urine drug screen was positive for cannabinoids, and blood alcohol levels were undetectable (< 10 mg/dL). A CT scan showed acute pancreatitis involving the tail and part of the pancreatic body, with edema and trace fluid around the pancreatic tail. Additionally, diminished density was noted in the pancreatic tail along with a small amount of ascites. An ultrasound showed no cholelithiasis or biliary ductal dilation. Serum IgG4 levels were normal (68 mg/dL; normal: 3-119 mg/dL). Initially, the patient denied medication use, smoking, or illicit drug use. Upon further questioning, he admitted to daily vaping, consuming 2 grams of THC liquid in 3-4 days, and occasional nicotine vaping. During his hospital stay, the patient was managed with intravenous fluids, pain management, and symptomatic treatment. He was subsequently discharged in a stable condition.
Discussion: This case involves a patient with symptoms, lab findings, and imaging suggestive of acute pancreatitis. There was no family history of hereditary pancreatitis, and common causes such as alcohol use, gallstones, hypertriglyceridemia, hypercalcemia, and autoimmune pancreatitis were ruled out. The patient's history was notable only for cannabis use. Based on the Naranjo algorithm, which yielded a score of six, the pancreatitis was considered possibly secondary to cannabis use. This report highlights potential gastrointestinal complications from cannabis consumption and underscores the need for healthcare providers to be aware of this possible adverse effect.
Disclosures:
Walaa Hasan, MD1, Aryeh Moskovits, DO2, Stephen Dimaggio, MD2, Farah Faridi, MD2. P3508 - From High to Harm: A Case of Cannabis-Induced Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Trinitas Regional Medical Center, Elizabeth, NJ; 2RWJ Barnabas Health, Trinitas Regional Medical Center, Elizabeth, NJ
Introduction: Cannabis consumption is increasing due to its legalization for medical and recreational use. While its effects on the central nervous system are well-known, its impact on other organ systems is less understood. This case report presents a rare instance of acute pancreatitis triggered by cannabis use.
Case Description/Methods: A 16-year-old male with no significant medical history presented with epigastric abdominal pain radiating to the back and vomiting. Physical examination revealed tenderness in the epigastric region and right upper quadrant. The patient was vitally stable. Initial lab results showed a white blood cell count of 15.3 x 10^3/μL and a lipase level of 152 U/L. His calcium level was 9.4 mg/dL, LDL was 113 mg/dL, and triglycerides were 40 mg/dL. A urine drug screen was positive for cannabinoids, and blood alcohol levels were undetectable (< 10 mg/dL). A CT scan showed acute pancreatitis involving the tail and part of the pancreatic body, with edema and trace fluid around the pancreatic tail. Additionally, diminished density was noted in the pancreatic tail along with a small amount of ascites. An ultrasound showed no cholelithiasis or biliary ductal dilation. Serum IgG4 levels were normal (68 mg/dL; normal: 3-119 mg/dL). Initially, the patient denied medication use, smoking, or illicit drug use. Upon further questioning, he admitted to daily vaping, consuming 2 grams of THC liquid in 3-4 days, and occasional nicotine vaping. During his hospital stay, the patient was managed with intravenous fluids, pain management, and symptomatic treatment. He was subsequently discharged in a stable condition.
Discussion: This case involves a patient with symptoms, lab findings, and imaging suggestive of acute pancreatitis. There was no family history of hereditary pancreatitis, and common causes such as alcohol use, gallstones, hypertriglyceridemia, hypercalcemia, and autoimmune pancreatitis were ruled out. The patient's history was notable only for cannabis use. Based on the Naranjo algorithm, which yielded a score of six, the pancreatitis was considered possibly secondary to cannabis use. This report highlights potential gastrointestinal complications from cannabis consumption and underscores the need for healthcare providers to be aware of this possible adverse effect.
Disclosures:
Walaa Hasan indicated no relevant financial relationships.
Aryeh Moskovits indicated no relevant financial relationships.
Stephen Dimaggio indicated no relevant financial relationships.
Farah Faridi indicated no relevant financial relationships.
Walaa Hasan, MD1, Aryeh Moskovits, DO2, Stephen Dimaggio, MD2, Farah Faridi, MD2. P3508 - From High to Harm: A Case of Cannabis-Induced Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
