Tuesday Poster Session
Category: Biliary/Pancreas
P3513 - The Unexpected GIST: Large Extra Gastrointestinal Stromal Tumor Mimicking a Pancreatic Neuroendocrine Tumor
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nadim A. Qadir, DO
University of Florida College of Medicine
Windermere, FL
Presenting Author(s)
Nadim A. Qadir, DO1, Anvit D. Reddy, DO2, Tara Kronen, DO, MA2, Laura Suzanne K. Suarez, MD2, Bruno Ribeiro, MD2
1University of Florida College of Medicine, Windermere, FL; 2University of Florida College of Medicine, Jacksonville, FL
Introduction: Gastro-intestinal stromal tumors (GISTs) were first thought to exclusively originate from mesodermal tissue from the interstitial cells of Cajal. Recent data has recognized that it can arise from multipotential mesenchymal stem cells. Approximately 60% occur within the stomach, and 35% in the small bowel. GISTs that originate outside the gastrointestinal tract such as the omentum, mesentery and retroperitoneum represent the remaining 5% and are defined as EGISTs. We present a patient who was thought to have a neuroendocrine tumor at the head of the pancreas and was later diagnosed with GIST.
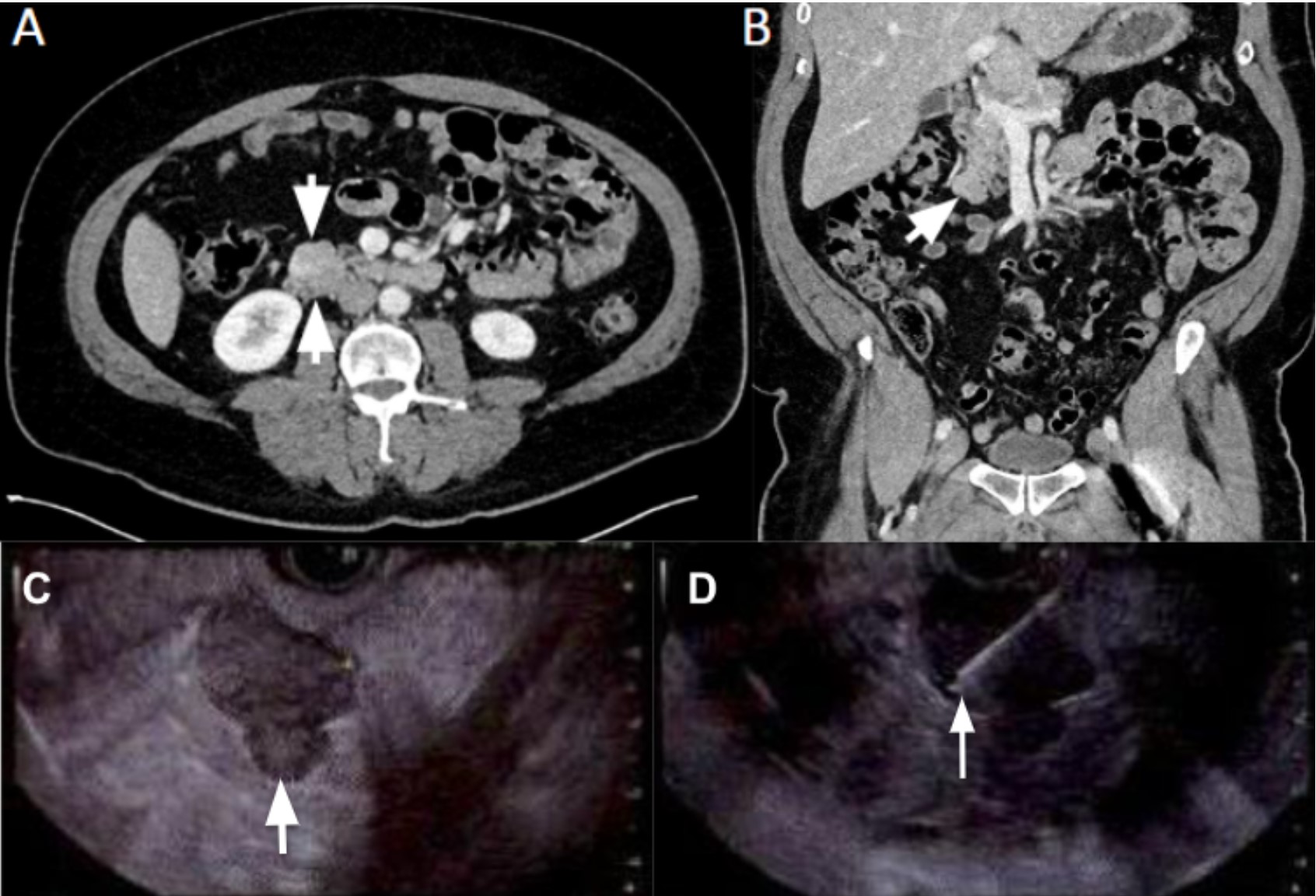
Case Description/Methods: A 53-year-old man with a medical history of diabetes mellitus type 2, hypertension, hyperlipidemia, and peptic ulcer disease presented to the hospital due to chest pain. He was at work moving palettes when he felt a sudden sharp epigastric and substernal chest pain with radiation down his left arm accompanied by left arm paresthesias with radiation to the back. Cardiac biomarkers and stress electrocardiogram were negative. Routine serology including lipase was unremarkable. Computed tomography angiogram (CTA) showed a 2.7 cm exophytic rounded focus adjacent to the head of the pancreas (Image 1A-1B). A magnetic resonance imaging (MRI) of the abdomen showed an enhancing pancreatic mass suggestive of a neuroendocrine tumor. Cancer tumor markers low. An endoscopic ultrasound (EUS) with fine needle biopsy was performed and a 21 mm by 28 mm mass at the uncinate process was found. Pathology reports confirmed GIST (Image 1C-1D). Immunostains CD117 were positive with S100 and SMA both negative. Surgical oncology recommended pancreaticoduodenectomy outpatient after medical optimization, and the patient was discharged in stable condition.
Discussion: Pancreatic EGISTs are extremely rare with only a few case reports in literature. The diagnosis of GIST is suggested by radiology however confirmation is based on histological, immunohistochemical, and molecular features (oncogenic c-Kit mutation). Tissue sampling is achieved with EUS with fine-needle biopsy. Standard treatment for primary GIST is complete surgical resection, where feasible, with the aim to obtain negative microscopic margins over the organ of origin. Imatinib has been shown to treat inoperable CD117 positive GIST's. In this patient, it was decided to pursue surgical resection due to the size and location of the GIST. Recurrence can occur, so more research is needed to establish surveillance guidelines after GIST resection.
Disclosures:
Nadim A. Qadir, DO1, Anvit D. Reddy, DO2, Tara Kronen, DO, MA2, Laura Suzanne K. Suarez, MD2, Bruno Ribeiro, MD2. P3513 - The Unexpected GIST: Large Extra Gastrointestinal Stromal Tumor Mimicking a Pancreatic Neuroendocrine Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Florida College of Medicine, Windermere, FL; 2University of Florida College of Medicine, Jacksonville, FL
Introduction: Gastro-intestinal stromal tumors (GISTs) were first thought to exclusively originate from mesodermal tissue from the interstitial cells of Cajal. Recent data has recognized that it can arise from multipotential mesenchymal stem cells. Approximately 60% occur within the stomach, and 35% in the small bowel. GISTs that originate outside the gastrointestinal tract such as the omentum, mesentery and retroperitoneum represent the remaining 5% and are defined as EGISTs. We present a patient who was thought to have a neuroendocrine tumor at the head of the pancreas and was later diagnosed with GIST.
Case Description/Methods: A 53-year-old man with a medical history of diabetes mellitus type 2, hypertension, hyperlipidemia, and peptic ulcer disease presented to the hospital due to chest pain. He was at work moving palettes when he felt a sudden sharp epigastric and substernal chest pain with radiation down his left arm accompanied by left arm paresthesias with radiation to the back. Cardiac biomarkers and stress electrocardiogram were negative. Routine serology including lipase was unremarkable. Computed tomography angiogram (CTA) showed a 2.7 cm exophytic rounded focus adjacent to the head of the pancreas (Image 1A-1B). A magnetic resonance imaging (MRI) of the abdomen showed an enhancing pancreatic mass suggestive of a neuroendocrine tumor. Cancer tumor markers low. An endoscopic ultrasound (EUS) with fine needle biopsy was performed and a 21 mm by 28 mm mass at the uncinate process was found. Pathology reports confirmed GIST (Image 1C-1D). Immunostains CD117 were positive with S100 and SMA both negative. Surgical oncology recommended pancreaticoduodenectomy outpatient after medical optimization, and the patient was discharged in stable condition.
Discussion: Pancreatic EGISTs are extremely rare with only a few case reports in literature. The diagnosis of GIST is suggested by radiology however confirmation is based on histological, immunohistochemical, and molecular features (oncogenic c-Kit mutation). Tissue sampling is achieved with EUS with fine-needle biopsy. Standard treatment for primary GIST is complete surgical resection, where feasible, with the aim to obtain negative microscopic margins over the organ of origin. Imatinib has been shown to treat inoperable CD117 positive GIST's. In this patient, it was decided to pursue surgical resection due to the size and location of the GIST. Recurrence can occur, so more research is needed to establish surveillance guidelines after GIST resection.
Figure: Image 1A-1B: Axial (A) and Coronal reformat (B) CT Images demonstrating an enhancing exophytic lobulated mass arising from the pancreatic head/uncinate process (white arrows) which causes mild mass effect upon the duodenum.
Image 1C-1D: (C) 21mm by 28mm uncinate mass seen; with features indicative of pancreatic neuroendocrine tumor. (D) Fine needle biopsy performed.
Image 1C-1D: (C) 21mm by 28mm uncinate mass seen; with features indicative of pancreatic neuroendocrine tumor. (D) Fine needle biopsy performed.
Disclosures:
Nadim Qadir indicated no relevant financial relationships.
Anvit Reddy indicated no relevant financial relationships.
Tara Kronen indicated no relevant financial relationships.
Laura Suzanne Suarez indicated no relevant financial relationships.
Bruno Ribeiro indicated no relevant financial relationships.
Nadim A. Qadir, DO1, Anvit D. Reddy, DO2, Tara Kronen, DO, MA2, Laura Suzanne K. Suarez, MD2, Bruno Ribeiro, MD2. P3513 - The Unexpected GIST: Large Extra Gastrointestinal Stromal Tumor Mimicking a Pancreatic Neuroendocrine Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
