Tuesday Poster Session
Category: Biliary/Pancreas
P3516 - Pancreaticopleural Fistula Presenting as a Hemothorax Stemming From Intraductal Papillary Mucinous Neoplasms
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RP
Rahul Patel, DO
Jefferson Health
Washington Township, NJ
Presenting Author(s)
Rahul Patel, DO1, Edward Bley, DO1, Marisa Pope, DO1, Christopher Chhoun, DO1, Joshua Soliman, DO1, C. Jonathan Foster, DO2
1Jefferson Health, Washington Township, NJ; 2Jefferson Health, Cherry Hill, NJ
Introduction: Pancreaticopleural fistula (PPF) is a rare entity that poses diagnostic and therapeutic challenges. We report a case of PPF presenting as a hemothorax in a patient without pancreatitis.
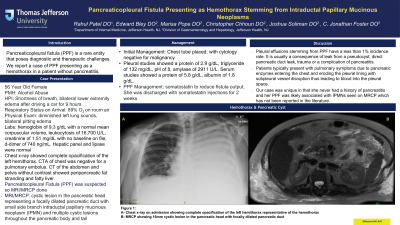
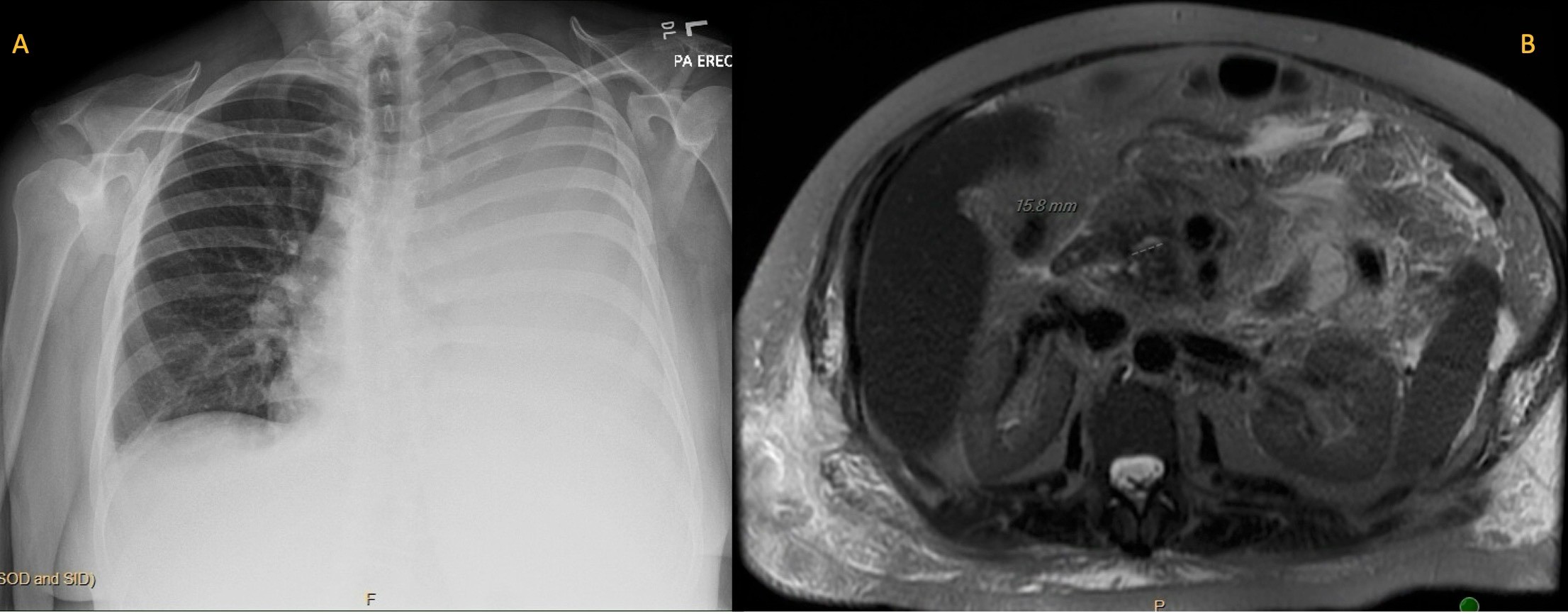
Case Description/Methods: A 56-year-old female with a history of alcohol abuse presented to the hospital with shortness of breath and bilateral lower extremity edema. Prior to arrival, she took a 9-hour car drive. She arrived with an oxygen saturation of 89%, so was placed on nasal cannula. Physical exam was pertinent for diminished left lung sounds and bilateral pitting edema. Lab work showed a hemoglobin of 9.3 g/dL with a normal mean corpuscular volume, leukocytosis of 16,700 U/L, creatinine of 1.51 mg/dL with no baseline on file, d-dimer of 740 ng/mL. Hepatic panel and lipase were normal. Chest x-ray showed complete opacification of the left hemithorax. CTA of chest was negative for a pulmonary embolus. CT of the abdomen and pelvis without contrast showed peripancreatic fat stranding and hepatic steatosis. A left sided chest tube was placed with 1300 cc of sanguineous fluid removed with pleural fluid cytology negative for malignancy. Pleural studies showed a protein of 2.9 g/dL, triglyceride of 132 mg/dL, pH of 8, amylase of 2911 U/L. Serum studies showed a protein of 5.8 g/dL, albumin of 1.8 g/dL. She did not meet criteria for pancreatitis but a PPF was suspected then confirmed with magnetic resonance cholangiopancreatography (MRCP) in order to evaluate pancreatic parenchyma and ductal anatomy. MRCP showed a cystic lesion in the pancreatic head representing a focally dilated pancreatic duct with small side branch intraductal papillary mucinous neoplasm (IPMN) and multiple cystic lesions throughout the pancreatic body and tail. She was started on somatostatin to reduce fistula output. At discharge, she was continued on somatostatin injections for 2 weeks and recommended for outpatient pancreatic lesion follow up.
Discussion: Pleural effusions from a PPF have a less than 1% incidence rate. The presentation of a hemothorax is even rarer. It is usually a consequence of leak from a pseudocyst, direct pancreatic duct leak, trauma or a complication of pancreatitis. Patients typically present with pulmonary symptoms due to pancreatic enzymes entering the chest and eroding the pleural lining with subpleural vessel disruption thus leading to blood into the pleural space. Our case was unique in that her PPF was associated with IPMNs which has not been reported in the literature and the presentation of a hemothorax.
Disclosures:
Rahul Patel, DO1, Edward Bley, DO1, Marisa Pope, DO1, Christopher Chhoun, DO1, Joshua Soliman, DO1, C. Jonathan Foster, DO2. P3516 - Pancreaticopleural Fistula Presenting as a Hemothorax Stemming From Intraductal Papillary Mucinous Neoplasms, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jefferson Health, Washington Township, NJ; 2Jefferson Health, Cherry Hill, NJ
Introduction: Pancreaticopleural fistula (PPF) is a rare entity that poses diagnostic and therapeutic challenges. We report a case of PPF presenting as a hemothorax in a patient without pancreatitis.
Case Description/Methods: A 56-year-old female with a history of alcohol abuse presented to the hospital with shortness of breath and bilateral lower extremity edema. Prior to arrival, she took a 9-hour car drive. She arrived with an oxygen saturation of 89%, so was placed on nasal cannula. Physical exam was pertinent for diminished left lung sounds and bilateral pitting edema. Lab work showed a hemoglobin of 9.3 g/dL with a normal mean corpuscular volume, leukocytosis of 16,700 U/L, creatinine of 1.51 mg/dL with no baseline on file, d-dimer of 740 ng/mL. Hepatic panel and lipase were normal. Chest x-ray showed complete opacification of the left hemithorax. CTA of chest was negative for a pulmonary embolus. CT of the abdomen and pelvis without contrast showed peripancreatic fat stranding and hepatic steatosis. A left sided chest tube was placed with 1300 cc of sanguineous fluid removed with pleural fluid cytology negative for malignancy. Pleural studies showed a protein of 2.9 g/dL, triglyceride of 132 mg/dL, pH of 8, amylase of 2911 U/L. Serum studies showed a protein of 5.8 g/dL, albumin of 1.8 g/dL. She did not meet criteria for pancreatitis but a PPF was suspected then confirmed with magnetic resonance cholangiopancreatography (MRCP) in order to evaluate pancreatic parenchyma and ductal anatomy. MRCP showed a cystic lesion in the pancreatic head representing a focally dilated pancreatic duct with small side branch intraductal papillary mucinous neoplasm (IPMN) and multiple cystic lesions throughout the pancreatic body and tail. She was started on somatostatin to reduce fistula output. At discharge, she was continued on somatostatin injections for 2 weeks and recommended for outpatient pancreatic lesion follow up.
Discussion: Pleural effusions from a PPF have a less than 1% incidence rate. The presentation of a hemothorax is even rarer. It is usually a consequence of leak from a pseudocyst, direct pancreatic duct leak, trauma or a complication of pancreatitis. Patients typically present with pulmonary symptoms due to pancreatic enzymes entering the chest and eroding the pleural lining with subpleural vessel disruption thus leading to blood into the pleural space. Our case was unique in that her PPF was associated with IPMNs which has not been reported in the literature and the presentation of a hemothorax.
Figure: Figure 1:
A- Chest x-ray on admission showing complete opacification of the left hemithorax representative of the hemothorax
B- MRCP showing 16mm cystic lesion in the pancreatic head with focally dilated pancreatic duct
A- Chest x-ray on admission showing complete opacification of the left hemithorax representative of the hemothorax
B- MRCP showing 16mm cystic lesion in the pancreatic head with focally dilated pancreatic duct
Disclosures:
Rahul Patel indicated no relevant financial relationships.
Edward Bley indicated no relevant financial relationships.
Marisa Pope indicated no relevant financial relationships.
Christopher Chhoun indicated no relevant financial relationships.
Joshua Soliman indicated no relevant financial relationships.
C. Jonathan Foster: Conmed – Consultant. Steris – Consultant.
Rahul Patel, DO1, Edward Bley, DO1, Marisa Pope, DO1, Christopher Chhoun, DO1, Joshua Soliman, DO1, C. Jonathan Foster, DO2. P3516 - Pancreaticopleural Fistula Presenting as a Hemothorax Stemming From Intraductal Papillary Mucinous Neoplasms, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
