Monday Poster Session
Category: Stomach
P3357 - Resolution of Gastric Adenocarcinoma After H. Pylori Eradication Alone
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- KL
Krystal Y. Lai, MD
University of Texas Southwestern
Dallas, TX
Presenting Author(s)
Award: Presidential Poster Award
Krystal Y. Lai, MD1, Lan Peng, MD1, Ariel W. Aday, MD2
1University of Texas Southwestern, Dallas, TX; 2UT Southwestern, Dallas, TX
Introduction: Gastric cancers (GC), of which >90% are gastric adenocarcinomas (GAC), rank 5th globally in cancer incidence and mortality. Pathogenesis of GC is a multifactorial process and one well-documented risk factor for its development is Helicobacter pylori infection. Eradication of H. pylori has been shown to reduce the incidence of GC but is not a therapeutic intervention for GC. Standard treatment for GC ranges from endoscopic resection in early-stage GC, to total gastrectomy, to systemic therapies for metastatic disease. If left untreated, GC is an aggressive disease with doubling times ranging from 11.8 months for early disease to 6.2 months for advanced disease. Here we present a case of biopsy-proven poorly differentiated GAC treated with no other therapy besides eradication of concurrently diagnosed H. Pylori.
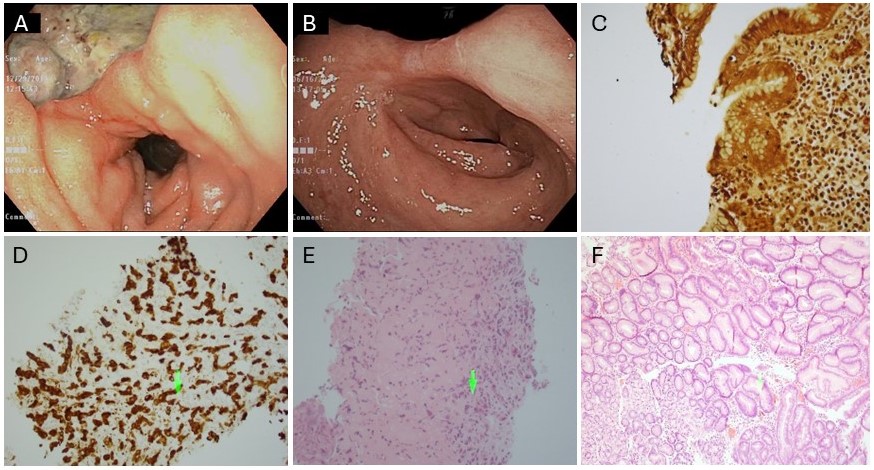
Case Description/Methods: A 66-year-old man with presented with cramping epigastric pain worse with meals. Labs were notable for a hemoglobin of 5.6 g/dL and dark stool on rectal exam. EGD showed a 4.5cm cratered gastric ulcer at the incisura. Pathology showed poorly differentiated GAC and H. pylori-associated gastritis with intestinal metaplasia. He completed a 14-day course of pantoprazole, amoxicillin, and clarithromycin before being lost to follow up. Six years later, the patient presented to the hospital for evaluation of an inguinal hernia. The gastroenterology team was consulted given his history of untreated GC. The patient denied any interim outpatient follow-up, chemotherapy, or surgical intervention for his GAC. EGD was performed which revealed a scar at the incisura at the site of the prior cancer. Biopsies showed mild chronic inactive gastritis with intestinal metaplasia, negative for H. pylori, dysplasia, or carcinoma.
Discussion: Though not fully understood, there is a clear relationship between H. Pylori infection and pathogenesis of GC. Not only does H. Pylori eradication decrease incidence of GC, but other studies suggest eradication provides further benefit even after diagnosis of GC, such as decreased incidence of metachronous GC after endoscopic resection, and improved survival benefit after gastrectomy. To our knowledge, there have been no other cases reported in the literature of GAC cure after H. pylori eradication alone. Mucosa-associated lymphoid tissue (MALT) lymphoma in the stomach is the only cancer for which H. Pylori eradication can be a first line therapy, but this case suggests that H. Pylori eradication may play an important role in treatment of other GCs.
Disclosures:
Krystal Y. Lai, MD1, Lan Peng, MD1, Ariel W. Aday, MD2. P3357 - Resolution of Gastric Adenocarcinoma After <i>H. Pylori</i> Eradication Alone, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Krystal Y. Lai, MD1, Lan Peng, MD1, Ariel W. Aday, MD2
1University of Texas Southwestern, Dallas, TX; 2UT Southwestern, Dallas, TX
Introduction: Gastric cancers (GC), of which >90% are gastric adenocarcinomas (GAC), rank 5th globally in cancer incidence and mortality. Pathogenesis of GC is a multifactorial process and one well-documented risk factor for its development is Helicobacter pylori infection. Eradication of H. pylori has been shown to reduce the incidence of GC but is not a therapeutic intervention for GC. Standard treatment for GC ranges from endoscopic resection in early-stage GC, to total gastrectomy, to systemic therapies for metastatic disease. If left untreated, GC is an aggressive disease with doubling times ranging from 11.8 months for early disease to 6.2 months for advanced disease. Here we present a case of biopsy-proven poorly differentiated GAC treated with no other therapy besides eradication of concurrently diagnosed H. Pylori.
Case Description/Methods: A 66-year-old man with presented with cramping epigastric pain worse with meals. Labs were notable for a hemoglobin of 5.6 g/dL and dark stool on rectal exam. EGD showed a 4.5cm cratered gastric ulcer at the incisura. Pathology showed poorly differentiated GAC and H. pylori-associated gastritis with intestinal metaplasia. He completed a 14-day course of pantoprazole, amoxicillin, and clarithromycin before being lost to follow up. Six years later, the patient presented to the hospital for evaluation of an inguinal hernia. The gastroenterology team was consulted given his history of untreated GC. The patient denied any interim outpatient follow-up, chemotherapy, or surgical intervention for his GAC. EGD was performed which revealed a scar at the incisura at the site of the prior cancer. Biopsies showed mild chronic inactive gastritis with intestinal metaplasia, negative for H. pylori, dysplasia, or carcinoma.
Discussion: Though not fully understood, there is a clear relationship between H. Pylori infection and pathogenesis of GC. Not only does H. Pylori eradication decrease incidence of GC, but other studies suggest eradication provides further benefit even after diagnosis of GC, such as decreased incidence of metachronous GC after endoscopic resection, and improved survival benefit after gastrectomy. To our knowledge, there have been no other cases reported in the literature of GAC cure after H. pylori eradication alone. Mucosa-associated lymphoid tissue (MALT) lymphoma in the stomach is the only cancer for which H. Pylori eradication can be a first line therapy, but this case suggests that H. Pylori eradication may play an important role in treatment of other GCs.
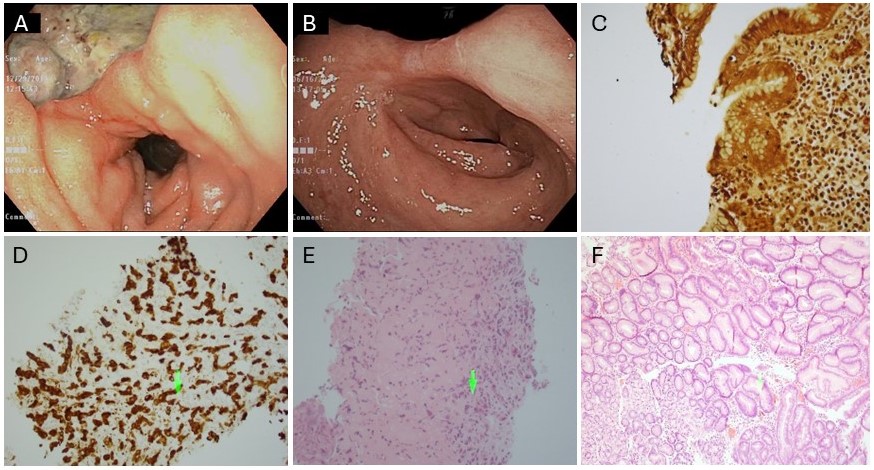
Figure: Figure 1. (A) Initial endoscopic image of large gastric ulcer at the incisura confirmed to be gastric adenocarcinoma on histology. (B) Follow up EGD 6 years after eradication of H. pylori showing resolution of ulcer and only residual scar remaining. (C) Histology of gastric ulcer biopsy from index endoscopy showing positive H. pylori by Warthin-Starry stain at 400x, (D) poorly differentiated adenocarcinoma confirmed by cytokeratin AE1/AE3 immunohistochemical stain at 200x and (E) poorly differentiated adenocarcinoma on H&E stain at 200x. (F) H&E stain of gastric biopsy following H. pylori eradication showing chronic inactive gastritis with intestinal metaplasia at 200x without any residual tumor cells.
Disclosures:
Krystal Lai indicated no relevant financial relationships.
Lan Peng indicated no relevant financial relationships.
Ariel Aday indicated no relevant financial relationships.
Krystal Y. Lai, MD1, Lan Peng, MD1, Ariel W. Aday, MD2. P3357 - Resolution of Gastric Adenocarcinoma After <i>H. Pylori</i> Eradication Alone, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

