Monday Poster Session
Category: Small Intestine
P3276 - Successful Medical Management of Intramural Duodenal Abscess
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AA
Ahmed Aref, MBBCh
Corewell Health William Beaumont University Hospital
Royal Oak, MI
Presenting Author(s)
Ahmed Aref, MBBCh1, Nazli Begum Ozturk, MD1, Laith H. Jamil, MD2
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Oakland University William Beaumont School of Medicine, Royal Oak, MI
Introduction: Intramural duodenal abscesses are rarely reported in literature, and are mostly caused by complications of a duodenal ulcer perforation. We present a case of intramural duodenal abscess in a patient with a complicated pancreatitis course.
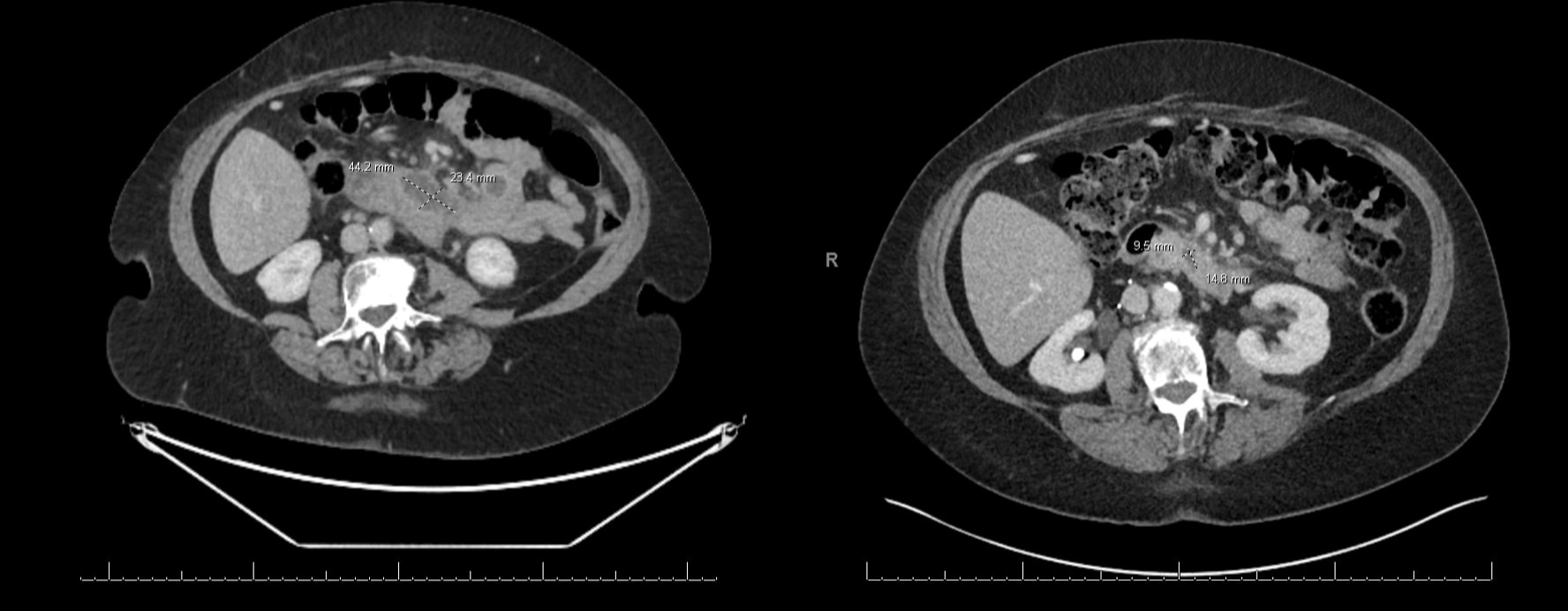
Case Description/Methods: We present a 71-year-old female with a past history of gallstone pancreatitis 3 years prior, complicated with infected necrosis, managed with cyst gastrostomy and necrosectomy. Course was also complicated with common bile duct stricture, choledocholithiasis requiring multiple endoscopic retrograde cholangio-panreatography (ERCP) procedures. She eventually underwent cholecystectomy 1.5 years prior to her current presentation to the emergency department (ED). She presented to the ED with epigastric pain, nausea and vomiting. In the ED, she was vitally stable and afebrile. Exam was notable for epigastric tenderness without peritoneal signs. Laboratory work-up was remarkable for WBC 11.6 bil/L (3.5-10.1 bil/L) with neutrophils 9.2 bil/L (1.6-7.2 bil/L). Blood cultures were negative. Computed tomography abdomen and pelvis (CTAP) with IV contrast showed a bilobed peripherally enhancing fluid collection within the third portion of the duodenum measuring 4.4 cm x 2.3 cm x 4.8 cm with surrounding fat stranding suggestive of an intramural abscess (Figure A). She was started on IV piperacillin-tazobactam and IV pantoprazole. Her symptoms completely resolved after 3 days and she was discharged with a 1-week course of oral amoxicillin-clavulanic acid and oral omeprazole with plan for repeat imaging. CTAP with IV contrast after 1 week showed near complete resolution of previously seen fluid collection with a minimal remaining fluid focus measuring 1.5 x 1 cm and decreased degree of surrounding inflammatory changes (Figure B). Endoscopic evaluation was not pursued given resolution of symptoms and significant improvement on surveillance imaging.
Discussion: There are no clear guidelines on the management of duodenal abscesses, and previously reported cases required endoscopic or surgical drainage. Our case highlights the successful management of duodenal abscess with antibiotic treatment without a need for an endoscopic procedure or drainage.
Disclosures:
Ahmed Aref, MBBCh1, Nazli Begum Ozturk, MD1, Laith H. Jamil, MD2. P3276 - Successful Medical Management of Intramural Duodenal Abscess, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Oakland University William Beaumont School of Medicine, Royal Oak, MI
Introduction: Intramural duodenal abscesses are rarely reported in literature, and are mostly caused by complications of a duodenal ulcer perforation. We present a case of intramural duodenal abscess in a patient with a complicated pancreatitis course.
Case Description/Methods: We present a 71-year-old female with a past history of gallstone pancreatitis 3 years prior, complicated with infected necrosis, managed with cyst gastrostomy and necrosectomy. Course was also complicated with common bile duct stricture, choledocholithiasis requiring multiple endoscopic retrograde cholangio-panreatography (ERCP) procedures. She eventually underwent cholecystectomy 1.5 years prior to her current presentation to the emergency department (ED). She presented to the ED with epigastric pain, nausea and vomiting. In the ED, she was vitally stable and afebrile. Exam was notable for epigastric tenderness without peritoneal signs. Laboratory work-up was remarkable for WBC 11.6 bil/L (3.5-10.1 bil/L) with neutrophils 9.2 bil/L (1.6-7.2 bil/L). Blood cultures were negative. Computed tomography abdomen and pelvis (CTAP) with IV contrast showed a bilobed peripherally enhancing fluid collection within the third portion of the duodenum measuring 4.4 cm x 2.3 cm x 4.8 cm with surrounding fat stranding suggestive of an intramural abscess (Figure A). She was started on IV piperacillin-tazobactam and IV pantoprazole. Her symptoms completely resolved after 3 days and she was discharged with a 1-week course of oral amoxicillin-clavulanic acid and oral omeprazole with plan for repeat imaging. CTAP with IV contrast after 1 week showed near complete resolution of previously seen fluid collection with a minimal remaining fluid focus measuring 1.5 x 1 cm and decreased degree of surrounding inflammatory changes (Figure B). Endoscopic evaluation was not pursued given resolution of symptoms and significant improvement on surveillance imaging.
Discussion: There are no clear guidelines on the management of duodenal abscesses, and previously reported cases required endoscopic or surgical drainage. Our case highlights the successful management of duodenal abscess with antibiotic treatment without a need for an endoscopic procedure or drainage.
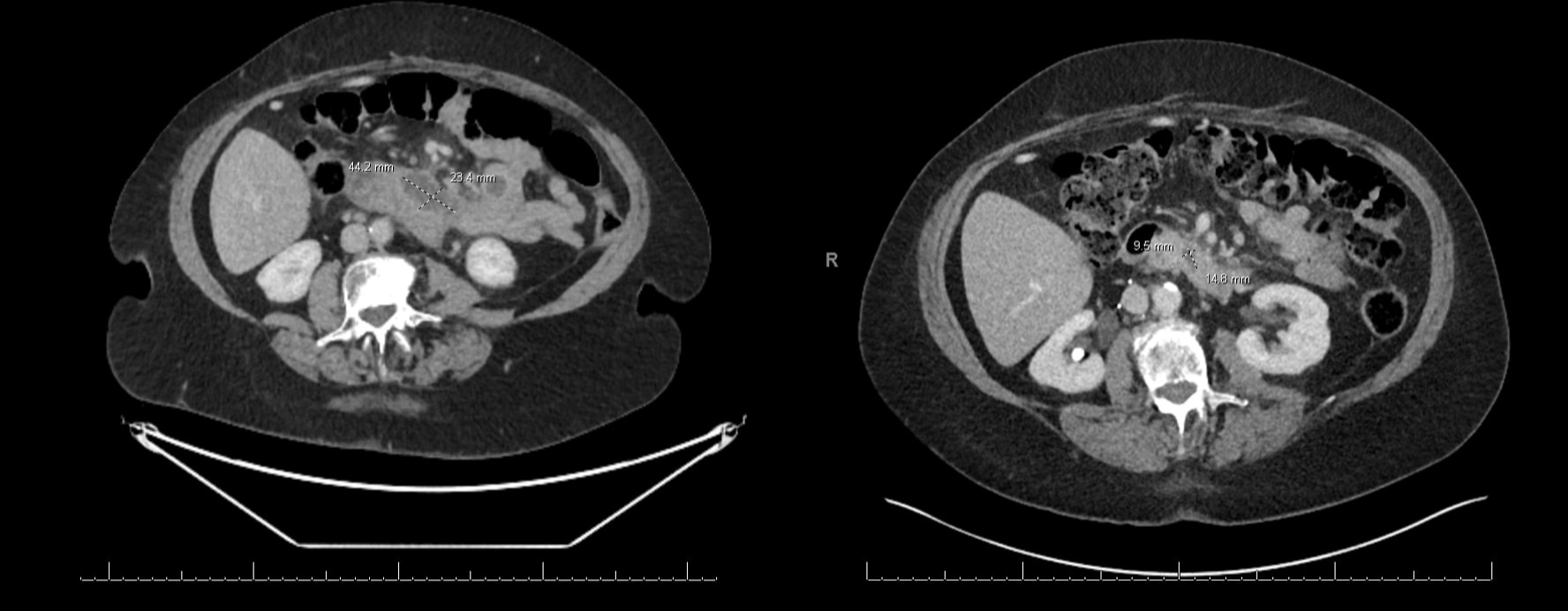
Figure: Initial (A) and post-treatment (B) CT scans.
Disclosures:
Ahmed Aref indicated no relevant financial relationships.
Nazli Begum Ozturk indicated no relevant financial relationships.
Laith Jamil indicated no relevant financial relationships.
Ahmed Aref, MBBCh1, Nazli Begum Ozturk, MD1, Laith H. Jamil, MD2. P3276 - Successful Medical Management of Intramural Duodenal Abscess, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
