Monday Poster Session
Category: Small Intestine
P3283 - Beyond the Surface: Metastatic Melanoma to the Small Intestine
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Catherine A. Loehr, MD
LSU
New Orleans, LA
Presenting Author(s)
Catherine Loehr, MD1, Salim C.. Lutfallah, BS2, Hunter Hall, MD1, Stephen Landreneau, MD1
1LSU, New Orleans, LA; 2LSU Health New Orleans School of Medicine, Metairie, LA
Introduction: Malignant melanoma, an epithelial cancer originating from melanocytes, can manifest in various tissue types. Metastatic melanoma can affect any major organ, often presenting with synchronous metastases. Common sites include the lungs, brain, liver, and gastrointestinal tract (GIT). Primary mucosal melanomas can also arise from various GI sites, including anorectal, oropharyngeal, small bowel, colon and esophagus.
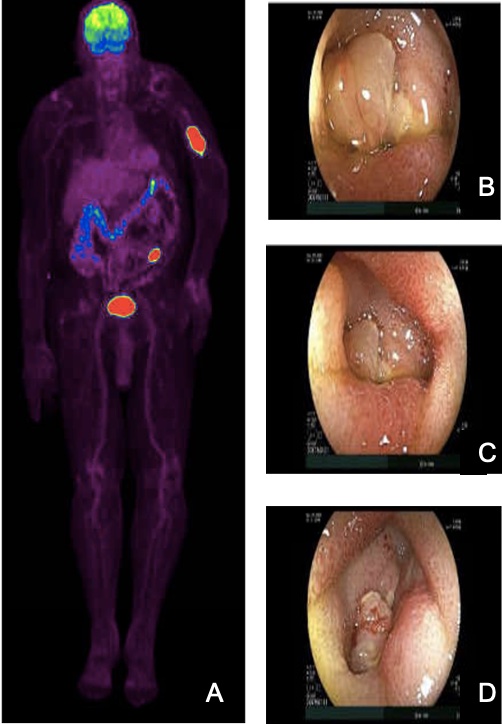
Case Description/Methods: A 78-year-old man, with a history of basal cell carcinoma of the nose, squamous cell carcinoma at multiple sites, and metastatic melanoma of the left humerus with an unknown primary status-post radiation, presented with fatigue, dyspnea on exertion, and a hemoglobin of 5.1. He denied overt signs of GI bleeding. Positron emission tomography (PET) revealed a hypermetabolic retroperitoneal lymph node with a focus in the jejunum, suggestive of intussusception without evidence of obstruction on computed tomography (CT). No definitive mass or concerning lead point was identified. Esophagogastroduodenoscopy was unremarkable, while colonoscopy demonstrated blood in the colon without a clear bleeding source. Video capsule endoscopy revealed blood in the proximal-mid small bowel and raised concern for capsule retention at an obstruction site resembling a small bowel mass. Double-balloon enteroscopy identified an ulcerated, pigmented, friable, mass in the distal jejunum without obstruction. Pathological examination confirmed the presence of malignant cells with enlarged nuclei, occasional intranuclear inclusions, and positive Melan-A and SOX10 immunostains. A final diagnosis of metastatic malignant melanoma was made.
Discussion: Metastatic melanoma frequently spreads to the GIT, clinically detected in only 2% but present in nearly 60% of autopsy cases of disseminated melanoma. The incidence of GI metastasis seems to be the highest in the jejunum and ileum. This may be attributed to the strong expression of CCR9, a chemokine receptor on melanoma cells, with its ligand, CCL25, highly expressed in the small intestine. The prognosis and management of the disease have been transformed by advancements in imaging, endoscopy, targeted systemic treatments such as immune checkpoint inhibitors and surgical interventions. In conclusion, metastatic melanoma involving the GIT should be considered as diagnosis can be challenging due to often subtle presentations and lack of GI-specific symptoms in many patients.
Disclosures:
Catherine Loehr, MD1, Salim C.. Lutfallah, BS2, Hunter Hall, MD1, Stephen Landreneau, MD1. P3283 - Beyond the Surface: Metastatic Melanoma to the Small Intestine, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1LSU, New Orleans, LA; 2LSU Health New Orleans School of Medicine, Metairie, LA
Introduction: Malignant melanoma, an epithelial cancer originating from melanocytes, can manifest in various tissue types. Metastatic melanoma can affect any major organ, often presenting with synchronous metastases. Common sites include the lungs, brain, liver, and gastrointestinal tract (GIT). Primary mucosal melanomas can also arise from various GI sites, including anorectal, oropharyngeal, small bowel, colon and esophagus.
Case Description/Methods: A 78-year-old man, with a history of basal cell carcinoma of the nose, squamous cell carcinoma at multiple sites, and metastatic melanoma of the left humerus with an unknown primary status-post radiation, presented with fatigue, dyspnea on exertion, and a hemoglobin of 5.1. He denied overt signs of GI bleeding. Positron emission tomography (PET) revealed a hypermetabolic retroperitoneal lymph node with a focus in the jejunum, suggestive of intussusception without evidence of obstruction on computed tomography (CT). No definitive mass or concerning lead point was identified. Esophagogastroduodenoscopy was unremarkable, while colonoscopy demonstrated blood in the colon without a clear bleeding source. Video capsule endoscopy revealed blood in the proximal-mid small bowel and raised concern for capsule retention at an obstruction site resembling a small bowel mass. Double-balloon enteroscopy identified an ulcerated, pigmented, friable, mass in the distal jejunum without obstruction. Pathological examination confirmed the presence of malignant cells with enlarged nuclei, occasional intranuclear inclusions, and positive Melan-A and SOX10 immunostains. A final diagnosis of metastatic malignant melanoma was made.
Discussion: Metastatic melanoma frequently spreads to the GIT, clinically detected in only 2% but present in nearly 60% of autopsy cases of disseminated melanoma. The incidence of GI metastasis seems to be the highest in the jejunum and ileum. This may be attributed to the strong expression of CCR9, a chemokine receptor on melanoma cells, with its ligand, CCL25, highly expressed in the small intestine. The prognosis and management of the disease have been transformed by advancements in imaging, endoscopy, targeted systemic treatments such as immune checkpoint inhibitors and surgical interventions. In conclusion, metastatic melanoma involving the GIT should be considered as diagnosis can be challenging due to often subtle presentations and lack of GI-specific symptoms in many patients.
Figure: Figure A. Positron emission tomography (PET) imaging revealed a hypermetabolic focus in a segment of the jejunum. Figure B, C, D. Mass in the jejunum seen on double-balloon enteroscopy.
Disclosures:
Catherine Loehr indicated no relevant financial relationships.
Salim Lutfallah indicated no relevant financial relationships.
Hunter Hall indicated no relevant financial relationships.
Stephen Landreneau indicated no relevant financial relationships.
Catherine Loehr, MD1, Salim C.. Lutfallah, BS2, Hunter Hall, MD1, Stephen Landreneau, MD1. P3283 - Beyond the Surface: Metastatic Melanoma to the Small Intestine, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
