Monday Poster Session
Category: Small Intestine
P3285 - Gastrointestinal Bleeding Due to IgA Vasculitis in an Elderly Individual – Recognition of Radiologic Features
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- NS
Nishali Shah, MD
Robert Wood Johnson Medical School, Rutgers University
New Brunswick, NJ
Presenting Author(s)
Award: Presidential Poster Award
Nishali Shah, MD, Ping He, MD, PhD, Pooja Jotwani, MD, Anish V. Patel, MD
Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: IgA vasculitis (IGAV) is an autoimmune condition caused by intravascular deposition of IgA immune complexes which manifests as cutaneous purpura, arthralgias, enteritis, and glomerulonephritis. IGAV is most commonly affects children < 20 years old, although it can rarely be seen in adults as well.
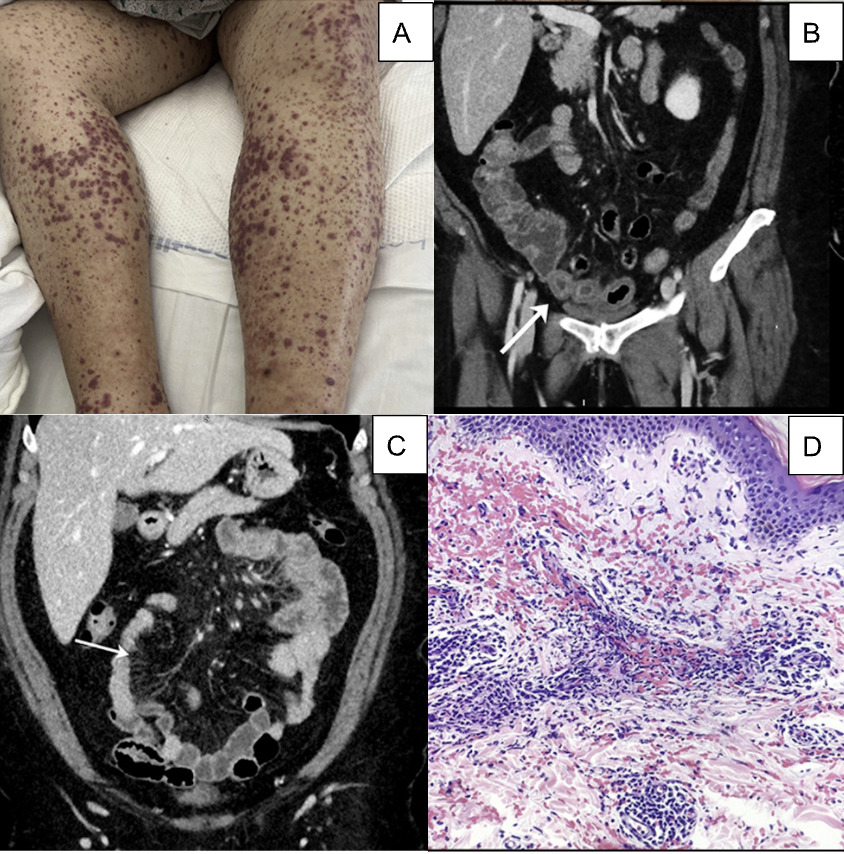
Case Description/Methods: A 63-year-old female with rheumatoid arthritis and hypertension presented to the hospital with a two-week history of progressive full-body rash, abdominal pain and hematochezia. On admission, physical exam was significant for palpable purpura over trunk and bilateral extremities (Figure 1A) and generalized abdominal tenderness. Admission hemoglobin was 14 g/dL and then later 11 g/dL. Creatinine was normal. CT scan of the abdomen revealed multiple areas of segmental wall thickening with “target signs” (Figure 1B) in the distal small bowel along with mesenteric vascular hyperemia (“comb sign”, Figure 1C) compatible with enteritis. Skin biopsy was performed that revealed leukocytoclastic vasculitis (Figure 1D), and the patient was diagnosed with IGAV. She was treated with a five-day course of intravenous steroids, which improved the abdominal pain, hematochezia and rash. EGD and colonoscopy were deferred due to improvement of symptoms. Upon discharge from the hospital, the patient was continued on oral steroids with rheumatology and gastroenterology follow-up where symptoms resolved.
Discussion: We present here an uncommon case of GI bleeding due to IGAV in an elderly patient. About 50% of patients with IGAV have GI involvement with enteritis. A study of 260 patients presenting with IGAV enteritis revealed that 99% had colicky abdominal pain, 31% had GI bleeding, 26% had diarrhea, and 4% had an acute surgical abdomen caused by intussusception and/or perforation (Audemard-Verger, 2020). GI involvement of IGAV can be diagnosed with abdominal CT or ultrasound imaging, which can show intestinal wall thickening with “target sign”, “comb sign” and lymphadenopathy. GI manifestations may precede purpura in IGAV, therefore the presence of “target” and “comb” signs in the imaging of patients with GI symptoms or acute abdomen should warrant a vigilant assessment and evaluation of dermatologic findings. If imaging is unrevealing, subsequent upper and lower endoscopy is performed to visualize ulcerations and biopsy for definitive diagnosis. In non-surgical cases, enteritis caused by IGAV is treated with intravenous and then oral steroids.
Disclosures:
Nishali Shah, MD, Ping He, MD, PhD, Pooja Jotwani, MD, Anish V. Patel, MD. P3285 - Gastrointestinal Bleeding Due to IgA Vasculitis in an Elderly Individual – Recognition of Radiologic Features, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Nishali Shah, MD, Ping He, MD, PhD, Pooja Jotwani, MD, Anish V. Patel, MD
Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: IgA vasculitis (IGAV) is an autoimmune condition caused by intravascular deposition of IgA immune complexes which manifests as cutaneous purpura, arthralgias, enteritis, and glomerulonephritis. IGAV is most commonly affects children < 20 years old, although it can rarely be seen in adults as well.
Case Description/Methods: A 63-year-old female with rheumatoid arthritis and hypertension presented to the hospital with a two-week history of progressive full-body rash, abdominal pain and hematochezia. On admission, physical exam was significant for palpable purpura over trunk and bilateral extremities (Figure 1A) and generalized abdominal tenderness. Admission hemoglobin was 14 g/dL and then later 11 g/dL. Creatinine was normal. CT scan of the abdomen revealed multiple areas of segmental wall thickening with “target signs” (Figure 1B) in the distal small bowel along with mesenteric vascular hyperemia (“comb sign”, Figure 1C) compatible with enteritis. Skin biopsy was performed that revealed leukocytoclastic vasculitis (Figure 1D), and the patient was diagnosed with IGAV. She was treated with a five-day course of intravenous steroids, which improved the abdominal pain, hematochezia and rash. EGD and colonoscopy were deferred due to improvement of symptoms. Upon discharge from the hospital, the patient was continued on oral steroids with rheumatology and gastroenterology follow-up where symptoms resolved.
Discussion: We present here an uncommon case of GI bleeding due to IGAV in an elderly patient. About 50% of patients with IGAV have GI involvement with enteritis. A study of 260 patients presenting with IGAV enteritis revealed that 99% had colicky abdominal pain, 31% had GI bleeding, 26% had diarrhea, and 4% had an acute surgical abdomen caused by intussusception and/or perforation (Audemard-Verger, 2020). GI involvement of IGAV can be diagnosed with abdominal CT or ultrasound imaging, which can show intestinal wall thickening with “target sign”, “comb sign” and lymphadenopathy. GI manifestations may precede purpura in IGAV, therefore the presence of “target” and “comb” signs in the imaging of patients with GI symptoms or acute abdomen should warrant a vigilant assessment and evaluation of dermatologic findings. If imaging is unrevealing, subsequent upper and lower endoscopy is performed to visualize ulcerations and biopsy for definitive diagnosis. In non-surgical cases, enteritis caused by IGAV is treated with intravenous and then oral steroids.
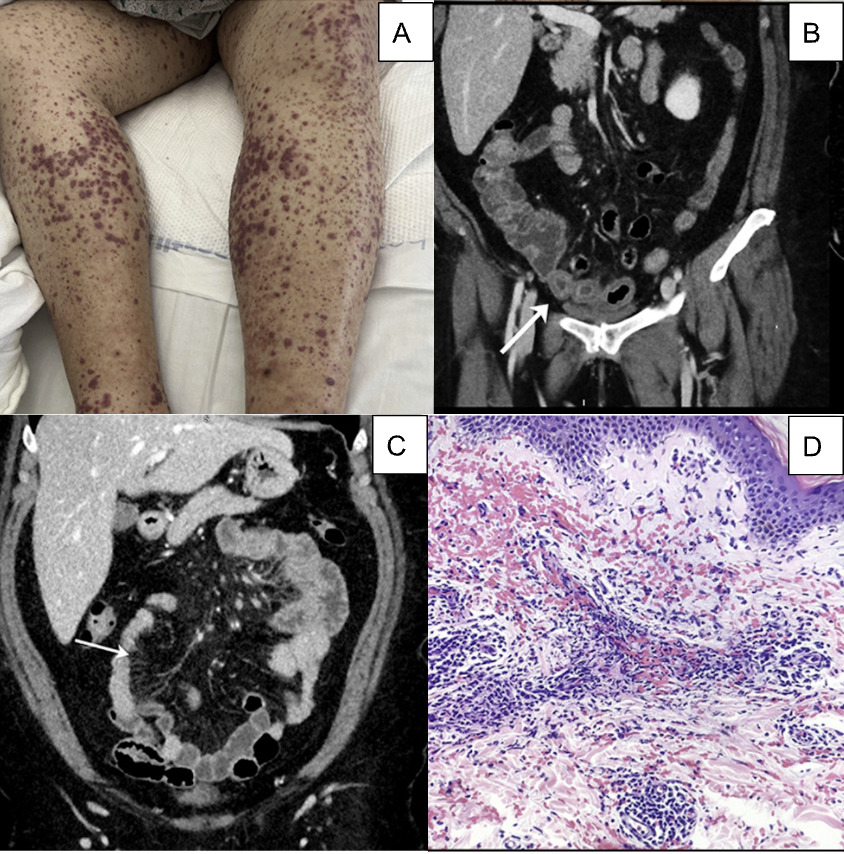
Figure: Figure 1. A) Palpable purpura over patient’s bilateral lower extremities. B) “Target sign” demonstrating areas of segmental wall thickening. C) “Comb sign” demonstrating hyperemia of mesenteric vessels. D) Skin biopsy with neutrophilic infiltration consistent with leukocytoclastic vasculitis.
Disclosures:
Nishali Shah indicated no relevant financial relationships.
Ping He indicated no relevant financial relationships.
Pooja Jotwani indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Nishali Shah, MD, Ping He, MD, PhD, Pooja Jotwani, MD, Anish V. Patel, MD. P3285 - Gastrointestinal Bleeding Due to IgA Vasculitis in an Elderly Individual – Recognition of Radiologic Features, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


