Monday Poster Session
Category: Small Intestine
P3214 - Safety and Efficacy of Endoscopic Mucosal Resection and Endoscopic Submucosal Dissection for Duodenal Neuroendocrine Tumors: A Systematic Review and Meta-Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- LT
Lyubov Tiegs, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Lyubov Tiegs, MD1, Amir Sultan Seid, MD1, Natalie Wilson, MD1, Nicole Theis-Mahon, 1, Rahul Karna, MD2, Mohammad Bilal, MD3
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
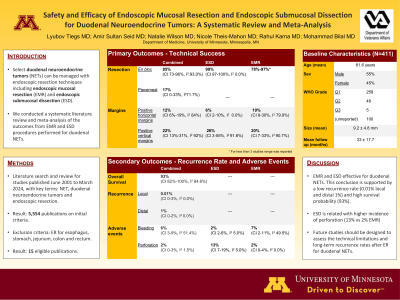
Introduction: Endoscopic resection (ER) techniques such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are being increasingly used for management of early gastrointestinal tract cancers and subepithelial lesions. Select duodenal neuroendocrine tumors (NETs) can be managed with ER due to low risk of lymph node and distant metastatic disease. We aim to conduct a systematic review and meta-analysis of outcomes of EMR and ESD performed for duodenal NETs.
Methods: We conducted a comprehensive literature search of multiple electronic databases from inception through May 2024 to identify studies assessing EMR and ESD of foregut NETs. Studies assessing ER for esophagus, stomach, jejunum, colon and rectum were excluded. Primary outcome was technical success and secondary outcomes were adverse events (AEs) and recurrence rate. Subgroup analysis was performed for EMR and ESD outcomes. A meta-analysis of proportions was performed for all outcomes.
Results: Out of 5,554 citations, 15 studies with 411 lesions of mean size 9.2 +/- 4.8 mm were included. The mean age was 61.6 years with 55% males. World Health Organization grade of tumor was G1/G2/G3: 258, 48, and 5 total, respectively. The pooled rate for total en-bloc resection was 85% (CI 73%-96%, I2: 93.0%), while the pooled rate for piecemeal resection was 17% (CI 0%-33%, I2 71.7%). Pooled rate for positive horizontal margins after resection was 12% (CI 6%-19%, I2 84.0%), and pooled rate for positive vertical margins after resection was 22% (CI 13%-31%, I2 91.8%). On histopathology, tumor invasion was found in mucosa in 55 total cases, submucosa 73 total cases, muscularis propria 2 cases and lymphovascular invasion 10 cases. Mean follow up duration was 33 +/- 17.7 months. Pooled proportion of local recurrence after EMR and ESD was 0.01% (CI 0%-3%, I2 0%), distal recurrence rate was 1% (0%-2% I2 0%), and overall survival rate was 93% (CI 82%-100%, I2 84.6%). Pooled rate of bleeding was 6% (CI 3%-9%, I2 51.4%), while pooled rate of perforation was 2% (CI 0%-3%, I2 1.5%). Table 1 shows subgroups analysis of outcomes when EMR and ESD was performed for duodenal NETs. ESD had higher rates of perforation as compared to EMR (13% vs 2%).
Discussion: We demonstrate that EMR and ESD effective for duodenal NETs, but ESD is related with higher incidence of perforation. Future studies should be designed to assess the technical limitations and long-term recurrence rates after ER for duodenal NETs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Lyubov Tiegs, MD1, Amir Sultan Seid, MD1, Natalie Wilson, MD1, Nicole Theis-Mahon, 1, Rahul Karna, MD2, Mohammad Bilal, MD3. P3214 - Safety and Efficacy of Endoscopic Mucosal Resection and Endoscopic Submucosal Dissection for Duodenal Neuroendocrine Tumors: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Endoscopic resection (ER) techniques such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are being increasingly used for management of early gastrointestinal tract cancers and subepithelial lesions. Select duodenal neuroendocrine tumors (NETs) can be managed with ER due to low risk of lymph node and distant metastatic disease. We aim to conduct a systematic review and meta-analysis of outcomes of EMR and ESD performed for duodenal NETs.
Methods: We conducted a comprehensive literature search of multiple electronic databases from inception through May 2024 to identify studies assessing EMR and ESD of foregut NETs. Studies assessing ER for esophagus, stomach, jejunum, colon and rectum were excluded. Primary outcome was technical success and secondary outcomes were adverse events (AEs) and recurrence rate. Subgroup analysis was performed for EMR and ESD outcomes. A meta-analysis of proportions was performed for all outcomes.
Results: Out of 5,554 citations, 15 studies with 411 lesions of mean size 9.2 +/- 4.8 mm were included. The mean age was 61.6 years with 55% males. World Health Organization grade of tumor was G1/G2/G3: 258, 48, and 5 total, respectively. The pooled rate for total en-bloc resection was 85% (CI 73%-96%, I2: 93.0%), while the pooled rate for piecemeal resection was 17% (CI 0%-33%, I2 71.7%). Pooled rate for positive horizontal margins after resection was 12% (CI 6%-19%, I2 84.0%), and pooled rate for positive vertical margins after resection was 22% (CI 13%-31%, I2 91.8%). On histopathology, tumor invasion was found in mucosa in 55 total cases, submucosa 73 total cases, muscularis propria 2 cases and lymphovascular invasion 10 cases. Mean follow up duration was 33 +/- 17.7 months. Pooled proportion of local recurrence after EMR and ESD was 0.01% (CI 0%-3%, I2 0%), distal recurrence rate was 1% (0%-2% I2 0%), and overall survival rate was 93% (CI 82%-100%, I2 84.6%). Pooled rate of bleeding was 6% (CI 3%-9%, I2 51.4%), while pooled rate of perforation was 2% (CI 0%-3%, I2 1.5%). Table 1 shows subgroups analysis of outcomes when EMR and ESD was performed for duodenal NETs. ESD had higher rates of perforation as compared to EMR (13% vs 2%).
Discussion: We demonstrate that EMR and ESD effective for duodenal NETs, but ESD is related with higher incidence of perforation. Future studies should be designed to assess the technical limitations and long-term recurrence rates after ER for duodenal NETs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Lyubov Tiegs indicated no relevant financial relationships.
Amir Sultan Seid indicated no relevant financial relationships.
Natalie Wilson indicated no relevant financial relationships.
Nicole Theis-Mahon indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Lyubov Tiegs, MD1, Amir Sultan Seid, MD1, Natalie Wilson, MD1, Nicole Theis-Mahon, 1, Rahul Karna, MD2, Mohammad Bilal, MD3. P3214 - Safety and Efficacy of Endoscopic Mucosal Resection and Endoscopic Submucosal Dissection for Duodenal Neuroendocrine Tumors: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
