Monday Poster Session
Category: Small Intestine
P3220 - Metastatic Lung Adenocarcinoma Resulting in Malignant Gastric Outlet Obstruction
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sravya Jannapureddy, MS, DO
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Sravya Jannapureddy, MS, DO1, Alexandra Kimchy, DO2, Mfoniso Umoren, MD, MHA1, Salima Mansoor Ali, MBBS1
1MedStar Georgetown University Hospital, Washington, DC; 2Georgetown University Hospital, Washington, DC
Introduction: The reported incidence of symptomatic gastrointestinal (GI) metastasis from primary lung malignancy is only 0.2 - 0.5%. Literature comparing histological subtypes of primary lung cancers found lung adenocarcinoma (LA) to exhibit the least propensity for GI metastasis. Within the small bowel, metastases localizing to the duodenum occur the least frequently. We detail an unusual case of malignant gastric outlet obstruction (GOO) from primary LA metastasizing to the duodenum.
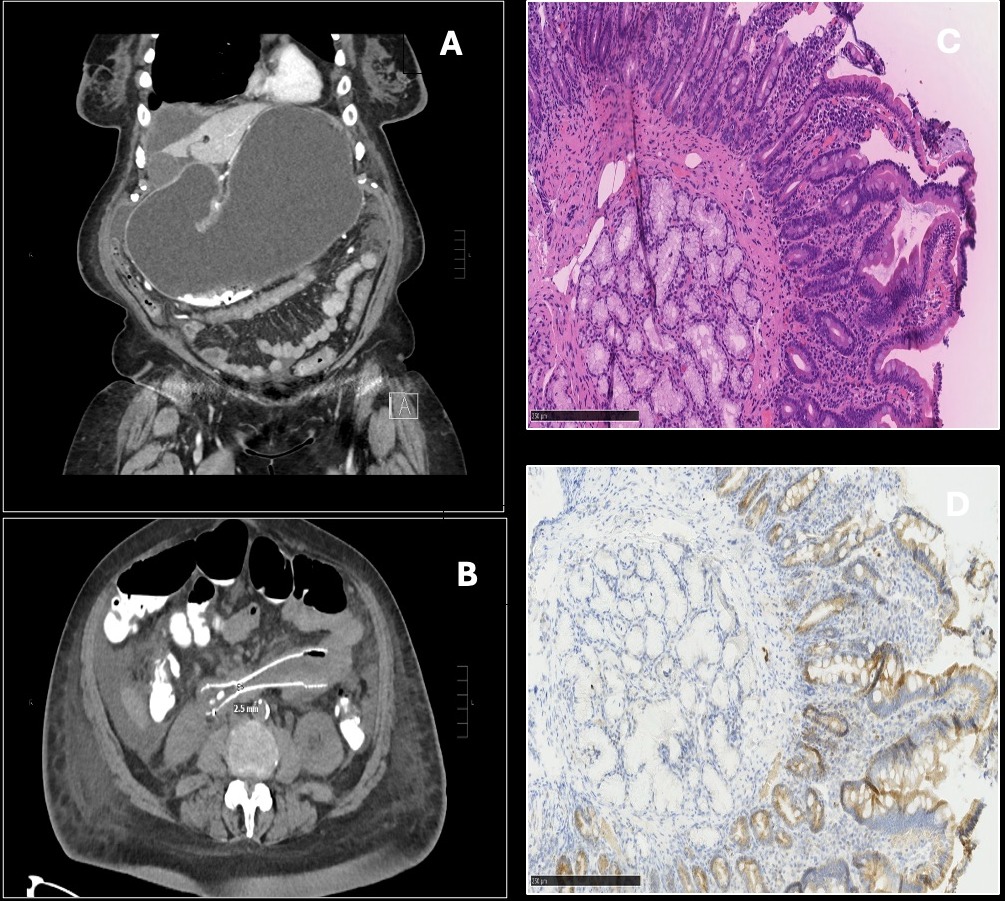
Case Description/Methods: An 81 year old female with stage IV LA on NVL-655, an enterally absorbed chemotherapy agent, presented with an 11 day history of intractable nausea and vomiting. CT Abdomen was significant for GOO at the third portion of the duodenum due to a lobulated soft tissue mass. Upper endoscopy revealed duodenal friability and a 4cm stricture extending from the distal end of descending duodenum (D2) to the proximal portion of the horizontal duodenum (D3). Biopsies were collected and a stent traversing the stricture was placed under endoscopic and fluoroscopic guidance. Three days after endoscopic stenting (ES), the patient’s symptoms recurred. A repeat CT confirmed stent failure with narrowing to 2.5mm. Her hospital course was further complicated by multi-organ deterioration including progression of her primary lung cancer with resultant respiratory failure, precluding laparoscopic gastrojejunostomy (LGJ). Ultimately, she was transitioned to comfort-focused care and passed shortly after. Duodenal biopsies eventually confirmed metastases from primary LA.
Discussion: Our case reinforces the debilitating consequences and therapeutic challenges of GOO secondary to a rare metastasis from primary LA. Disruption in chemotherapy due to GOO and failed interventions may result in disease progression and increases morbidity in an already fragile patient population. ES and LGJ, the two prevailing treatments for malignant GOO, either provide inconsistent relief of the obstruction or are associated with higher costs, longer recovery times, and significant adverse events. Endoscopic ultrasound-guided gastroenterostomy (EUS-GE) is a minimally invasive alternative that combines the reduced risk of re-obstruction offered by LGJ with the rapid symptomatic relief and cost benefits of ES. Future studies leading to standardization of EUS-GE may result in improved outcomes for patients with malignant GOO and provide a therapeutic option for those considered poor surgical candidates who experience stent failure.
Disclosures:
Sravya Jannapureddy, MS, DO1, Alexandra Kimchy, DO2, Mfoniso Umoren, MD, MHA1, Salima Mansoor Ali, MBBS1. P3220 - Metastatic Lung Adenocarcinoma Resulting in Malignant Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MedStar Georgetown University Hospital, Washington, DC; 2Georgetown University Hospital, Washington, DC
Introduction: The reported incidence of symptomatic gastrointestinal (GI) metastasis from primary lung malignancy is only 0.2 - 0.5%. Literature comparing histological subtypes of primary lung cancers found lung adenocarcinoma (LA) to exhibit the least propensity for GI metastasis. Within the small bowel, metastases localizing to the duodenum occur the least frequently. We detail an unusual case of malignant gastric outlet obstruction (GOO) from primary LA metastasizing to the duodenum.
Case Description/Methods: An 81 year old female with stage IV LA on NVL-655, an enterally absorbed chemotherapy agent, presented with an 11 day history of intractable nausea and vomiting. CT Abdomen was significant for GOO at the third portion of the duodenum due to a lobulated soft tissue mass. Upper endoscopy revealed duodenal friability and a 4cm stricture extending from the distal end of descending duodenum (D2) to the proximal portion of the horizontal duodenum (D3). Biopsies were collected and a stent traversing the stricture was placed under endoscopic and fluoroscopic guidance. Three days after endoscopic stenting (ES), the patient’s symptoms recurred. A repeat CT confirmed stent failure with narrowing to 2.5mm. Her hospital course was further complicated by multi-organ deterioration including progression of her primary lung cancer with resultant respiratory failure, precluding laparoscopic gastrojejunostomy (LGJ). Ultimately, she was transitioned to comfort-focused care and passed shortly after. Duodenal biopsies eventually confirmed metastases from primary LA.
Discussion: Our case reinforces the debilitating consequences and therapeutic challenges of GOO secondary to a rare metastasis from primary LA. Disruption in chemotherapy due to GOO and failed interventions may result in disease progression and increases morbidity in an already fragile patient population. ES and LGJ, the two prevailing treatments for malignant GOO, either provide inconsistent relief of the obstruction or are associated with higher costs, longer recovery times, and significant adverse events. Endoscopic ultrasound-guided gastroenterostomy (EUS-GE) is a minimally invasive alternative that combines the reduced risk of re-obstruction offered by LGJ with the rapid symptomatic relief and cost benefits of ES. Future studies leading to standardization of EUS-GE may result in improved outcomes for patients with malignant GOO and provide a therapeutic option for those considered poor surgical candidates who experience stent failure.
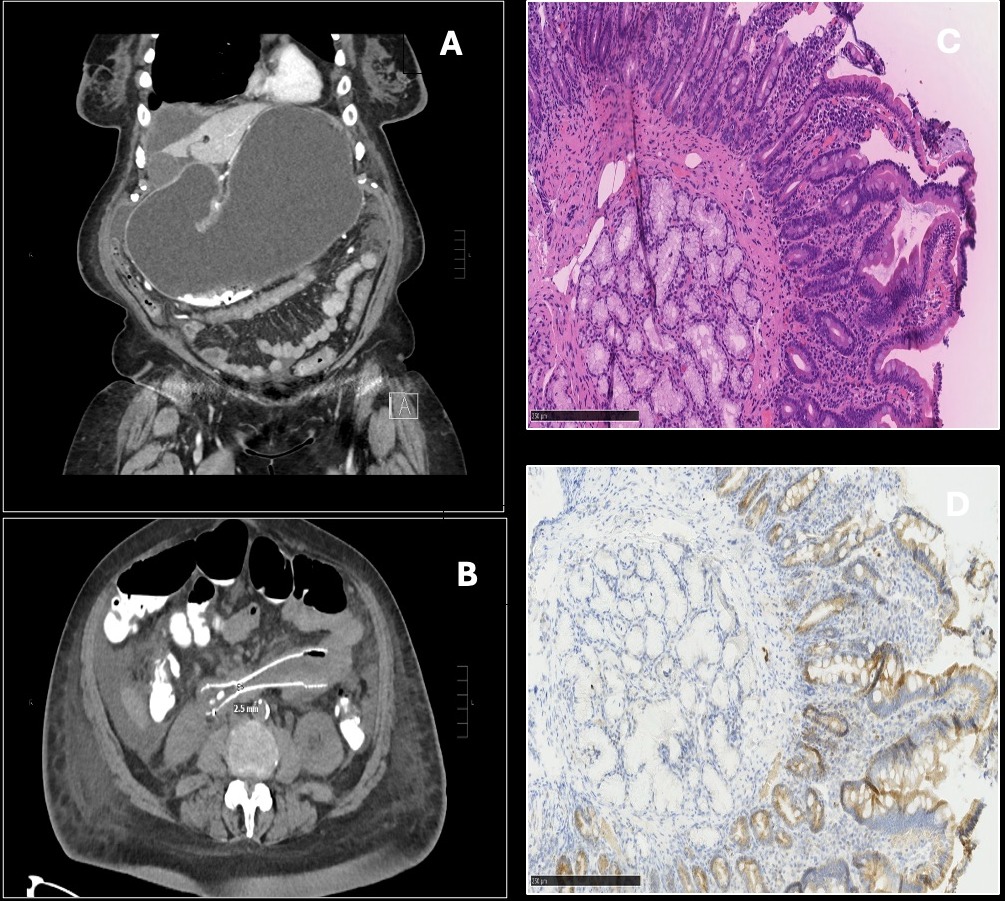
Figure: A, CT showing significantly distended stomach. B, Post-ES CT demonstrating focal narrowing at site of duodenal stent to 2.5mm. C, H&E stain of duodenal biopsy showing a small cluster of neoplastic cells within the lymphatics. D, TTF-1 stain confirming neoplastic cells were of pulmonary origin.
Disclosures:
Sravya Jannapureddy indicated no relevant financial relationships.
Alexandra Kimchy indicated no relevant financial relationships.
Mfoniso Umoren indicated no relevant financial relationships.
Salima Mansoor Ali indicated no relevant financial relationships.
Sravya Jannapureddy, MS, DO1, Alexandra Kimchy, DO2, Mfoniso Umoren, MD, MHA1, Salima Mansoor Ali, MBBS1. P3220 - Metastatic Lung Adenocarcinoma Resulting in Malignant Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
