Monday Poster Session
Category: Small Intestine
P3228 - A Rare Case of Collagenous Duodenitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Monica Arora, DO
Northwell Health Mather Hospital
Middle Island, NY
Presenting Author(s)
Award: Presidential Poster Award
Monica Arora, DO1, Muhammad Jahanzaib Khan, MD2, Ramona Rajapakse, MD3
1Northwell Health Mather Hospital, Middle Island, NY; 2Mather Hospital, Northwell Health, New York, NY; 3Mather Hospital, Northwell Health, Port Jefferson, NY
Introduction: Collagenous duodenitis is a rare disorder characterized by significant subepithelial collagen deposition and mucosal inflammation within the duodenum. While documented cases reveal associations with collagenous colitis or collagenous gastritis, only two instances of isolated collagenous duodenitis without colonic involvement have been reported to date.
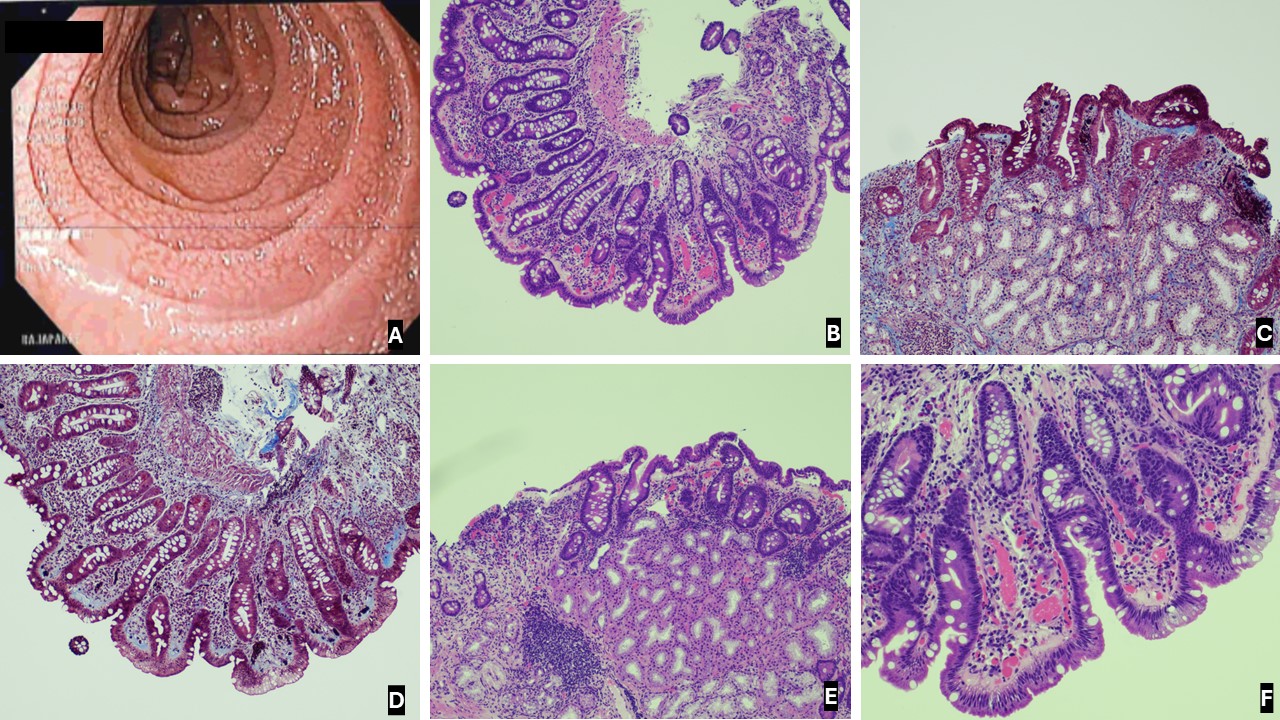
Case Description/Methods: An 87-year-old female with a history of transient ischemic attack, chronic kidney disease, reflux, and iron deficiency anemia presented with persistent dysphagia to solids, intermittent non-radiating epigastric pain, decreased oral intake, weight loss, and fatigue. She denied nausea, vomiting, melena, hematochezia, diarrhea, or constipation. Labs showed anemia (Hgb 9.5), while the rest of the investigations, including CT abdomen, were unremarkable. Celiac workup was negative. A routine colonoscopy in 2015 was also unremarkable. An EGD revealed a marked scalloped appearance of the duodenal bulb and the second portion of the duodenum. Pathology revealed duodenal mucosa with complete villous atrophy and a thickened subepithelial collagen band, consistent with collagenous duodenitis.
Discussion: The clinical, endoscopic, and histologic features of collagenous gastroenteritides are well-established. However, involvement of the duodenum, known as collagenous duodenitis, is exceptionally rare, especially without colonic involvement. Clinical presentations vary depending on the affected gastrointestinal region. Collagenous duodenitis often manifests as chronic watery diarrhea and weight loss secondary to concurrent collagenous colitis. Our patient’s presenting symptoms were atypical in comparison.
EGD may reveal findings similar to celiac sprue - villous atrophy or scalloped appearance of the duodenal mucosa, as observed in our case. Diagnosis relies on distinct histology, with subepithelial collagen bands measuring 10 mm in thickness.
The etiology of collagenous duodenitis remains poorly understood. Proposed hypotheses include chronic inflammation, autoimmunity and leakage of plasma protein, fibrinogen leading to collagen replacement. Collagen deposition is a reparative process responding to inflammatory, infectious, or toxic damage. No established treatment protocols exist for collagenous gastroenteritides. Therapies, such as corticosteroids, ranitidine, omeprazole, misoprostol, sucralfate, aminosalicylates, sulfasalazine, cholestyramine, and hypoallergenic diets, have demonstrated marginal results.
Disclosures:
Monica Arora, DO1, Muhammad Jahanzaib Khan, MD2, Ramona Rajapakse, MD3. P3228 - A Rare Case of Collagenous Duodenitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Monica Arora, DO1, Muhammad Jahanzaib Khan, MD2, Ramona Rajapakse, MD3
1Northwell Health Mather Hospital, Middle Island, NY; 2Mather Hospital, Northwell Health, New York, NY; 3Mather Hospital, Northwell Health, Port Jefferson, NY
Introduction: Collagenous duodenitis is a rare disorder characterized by significant subepithelial collagen deposition and mucosal inflammation within the duodenum. While documented cases reveal associations with collagenous colitis or collagenous gastritis, only two instances of isolated collagenous duodenitis without colonic involvement have been reported to date.
Case Description/Methods: An 87-year-old female with a history of transient ischemic attack, chronic kidney disease, reflux, and iron deficiency anemia presented with persistent dysphagia to solids, intermittent non-radiating epigastric pain, decreased oral intake, weight loss, and fatigue. She denied nausea, vomiting, melena, hematochezia, diarrhea, or constipation. Labs showed anemia (Hgb 9.5), while the rest of the investigations, including CT abdomen, were unremarkable. Celiac workup was negative. A routine colonoscopy in 2015 was also unremarkable. An EGD revealed a marked scalloped appearance of the duodenal bulb and the second portion of the duodenum. Pathology revealed duodenal mucosa with complete villous atrophy and a thickened subepithelial collagen band, consistent with collagenous duodenitis.
Discussion: The clinical, endoscopic, and histologic features of collagenous gastroenteritides are well-established. However, involvement of the duodenum, known as collagenous duodenitis, is exceptionally rare, especially without colonic involvement. Clinical presentations vary depending on the affected gastrointestinal region. Collagenous duodenitis often manifests as chronic watery diarrhea and weight loss secondary to concurrent collagenous colitis. Our patient’s presenting symptoms were atypical in comparison.
EGD may reveal findings similar to celiac sprue - villous atrophy or scalloped appearance of the duodenal mucosa, as observed in our case. Diagnosis relies on distinct histology, with subepithelial collagen bands measuring 10 mm in thickness.
The etiology of collagenous duodenitis remains poorly understood. Proposed hypotheses include chronic inflammation, autoimmunity and leakage of plasma protein, fibrinogen leading to collagen replacement. Collagen deposition is a reparative process responding to inflammatory, infectious, or toxic damage. No established treatment protocols exist for collagenous gastroenteritides. Therapies, such as corticosteroids, ranitidine, omeprazole, misoprostol, sucralfate, aminosalicylates, sulfasalazine, cholestyramine, and hypoallergenic diets, have demonstrated marginal results.
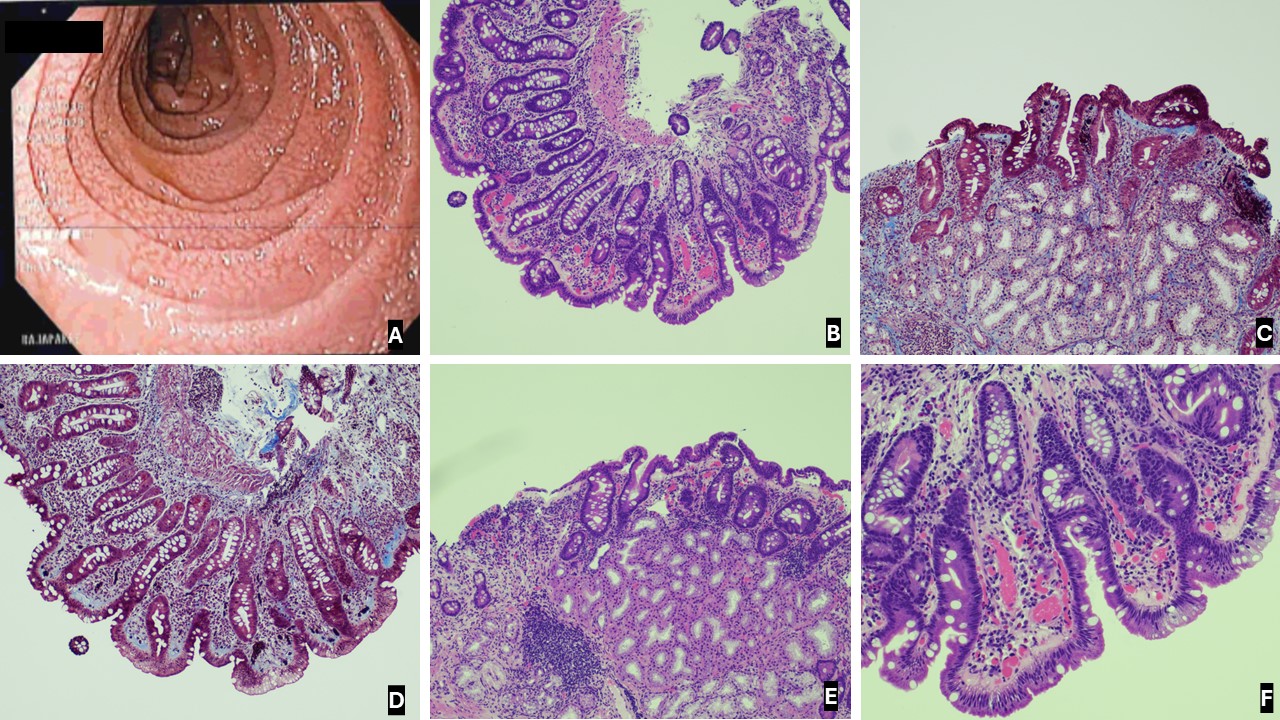
Figure: Figure A: Scalloped duodenum on endoscopy.
Figure B, C, D, E, F: Duodenal mucosa with marked villous atrophy and a thickened subepithelial collagen band (light pink on the H&E images, blue on the trichrome images) that is entrapping blood vessels and fibroblasts.
Figure B, C, D, E, F: Duodenal mucosa with marked villous atrophy and a thickened subepithelial collagen band (light pink on the H&E images, blue on the trichrome images) that is entrapping blood vessels and fibroblasts.
Disclosures:
Monica Arora indicated no relevant financial relationships.
Muhammad Jahanzaib Khan indicated no relevant financial relationships.
Ramona Rajapakse indicated no relevant financial relationships.
Monica Arora, DO1, Muhammad Jahanzaib Khan, MD2, Ramona Rajapakse, MD3. P3228 - A Rare Case of Collagenous Duodenitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

