Monday Poster Session
Category: Liver
P3156 - Direct Visualization of Hepatocellular Carcinoma with Complete Bile Duct Invasion Using Peroral Cholangioscopy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Fadi Dahoud, BS
David Geffen School of Medicine at UCLA
Los Angeles, CA
Presenting Author(s)
Fadi Dahoud, BS1, Elizza E. Villarruel, BS2, Hellen Jumo, BSc1, Lavender Micalo, BS1, Laura Mcenerney, MD3, Danny Issa, MD1
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, La Puente, CA; 3David Geffen School of Medicine at UCLA, Santa Clarita, CA
Introduction: Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer, constituting up to 90% of cases. While most tumors originate from hepatocytes, a subset of HCCs originating from the biliary epithelial cells has been reported and is exceedingly rare. Here, we present a very rare case of HCC causing complete invasion into the intra-hepatic bile ducts and review the diagnostic method.
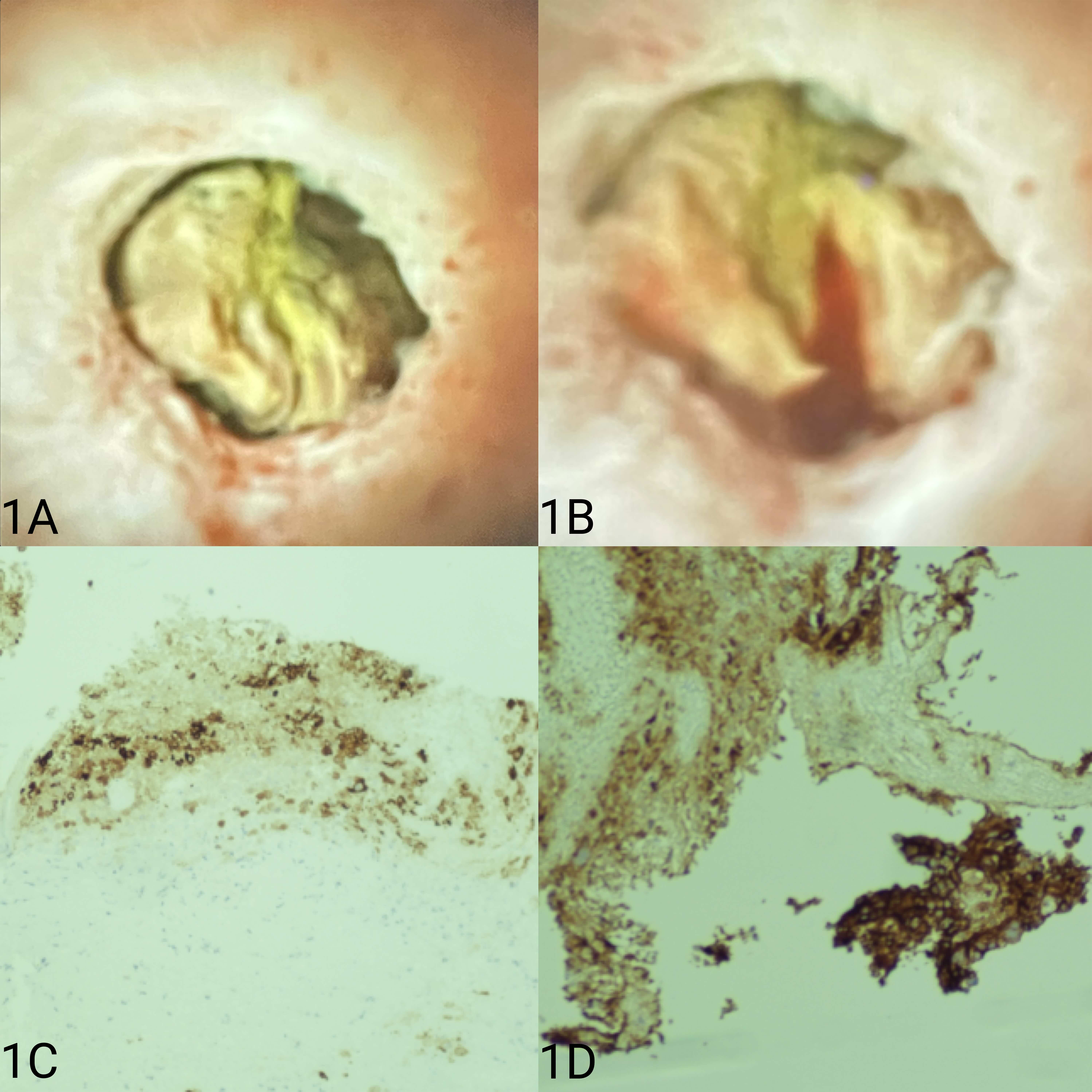
Case Description/Methods: A 66 year-old man with long-standing untreated chronic hepatitis C, type 2 diabetes and recently diagnosed cirrhosis presented with acute RUQ abdominal pain associated with poor oral intake. He described a weight loss of 10 lbs. over 3 months. He underwent a CT scan that revealed liver cirrhosis, a mass in liver segment 8, and portal vein thrombosis. His labs were unremarkable except for elevated hepatitis C RNA level at 1,990,000 IU/mL. Subsequently, a multiphase CT did not demonstrate characteristic findings for HCC. An MRCP revealed an intrahepatic biliary stricture caused by the mass with upstream dilatation. ERCP with the single-operator cholangioscopy revealed a tumor invasion into the right main intrahepatic duct with a complete cut-off of the duct. Direct visualization was concerning for malignancy (Image 1A, B). Cholangioscopy biopsies underwent morphology and immunohistochemical examinations and showed HCC staining for Pancytokeratin, Glypican-3, and cytoskeletal (CK)19 originating from the bile ducts, suggesting a biliary type of HCC (Image 1C, D). The mass was outside Milan criteria, and the patient was started on atezolizumab/bevacizumab therapy. His liver functions worsened rapidly, and he expired 2 months after his presentation.
Discussion: Aggressive HCC tumors can invade into the bile ducts and pose a diagnostic challenge. Imaging modalities may not be accurate in the distinction of bile duct from conventional HCC, and tumor markers such as alpha-fetoprotein, portal vein tumor thrombus, or peripheral blood neutrophil-to-lymphocyte ratio may not be elevated as in our patient. The definitive diagnosis often relies on biopsy followed by histopathological exam and staining. Cholangioscopy during ERCP allows for a high-quality examination and adequate tissue acquisition with the new improved forceps. Caution is advised as this tumor bleeds even with gentle biopsy (Image 1B). The combination of atezolizumab (PD-L1 inhibitor) and bevacizumab has shown to be relatively effective. Overall, the prognosis remains poor, and early detection of this disease is essential.
Disclosures:
Fadi Dahoud, BS1, Elizza E. Villarruel, BS2, Hellen Jumo, BSc1, Lavender Micalo, BS1, Laura Mcenerney, MD3, Danny Issa, MD1. P3156 - Direct Visualization of Hepatocellular Carcinoma with Complete Bile Duct Invasion Using Peroral Cholangioscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, La Puente, CA; 3David Geffen School of Medicine at UCLA, Santa Clarita, CA
Introduction: Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer, constituting up to 90% of cases. While most tumors originate from hepatocytes, a subset of HCCs originating from the biliary epithelial cells has been reported and is exceedingly rare. Here, we present a very rare case of HCC causing complete invasion into the intra-hepatic bile ducts and review the diagnostic method.
Case Description/Methods: A 66 year-old man with long-standing untreated chronic hepatitis C, type 2 diabetes and recently diagnosed cirrhosis presented with acute RUQ abdominal pain associated with poor oral intake. He described a weight loss of 10 lbs. over 3 months. He underwent a CT scan that revealed liver cirrhosis, a mass in liver segment 8, and portal vein thrombosis. His labs were unremarkable except for elevated hepatitis C RNA level at 1,990,000 IU/mL. Subsequently, a multiphase CT did not demonstrate characteristic findings for HCC. An MRCP revealed an intrahepatic biliary stricture caused by the mass with upstream dilatation. ERCP with the single-operator cholangioscopy revealed a tumor invasion into the right main intrahepatic duct with a complete cut-off of the duct. Direct visualization was concerning for malignancy (Image 1A, B). Cholangioscopy biopsies underwent morphology and immunohistochemical examinations and showed HCC staining for Pancytokeratin, Glypican-3, and cytoskeletal (CK)19 originating from the bile ducts, suggesting a biliary type of HCC (Image 1C, D). The mass was outside Milan criteria, and the patient was started on atezolizumab/bevacizumab therapy. His liver functions worsened rapidly, and he expired 2 months after his presentation.
Discussion: Aggressive HCC tumors can invade into the bile ducts and pose a diagnostic challenge. Imaging modalities may not be accurate in the distinction of bile duct from conventional HCC, and tumor markers such as alpha-fetoprotein, portal vein tumor thrombus, or peripheral blood neutrophil-to-lymphocyte ratio may not be elevated as in our patient. The definitive diagnosis often relies on biopsy followed by histopathological exam and staining. Cholangioscopy during ERCP allows for a high-quality examination and adequate tissue acquisition with the new improved forceps. Caution is advised as this tumor bleeds even with gentle biopsy (Image 1B). The combination of atezolizumab (PD-L1 inhibitor) and bevacizumab has shown to be relatively effective. Overall, the prognosis remains poor, and early detection of this disease is essential.
Figure: Peroral cholangioscopy revealed a floating, partially exposed tumor tissue with cut-off of the intrahepatic bile duct the easily bleed upon contact (A, B).Tumor cells were immunohistochemically positive for hepatocyte Glypivcan-3 (C) and for cytokeratin 19 (D).
Disclosures:
Fadi Dahoud indicated no relevant financial relationships.
Elizza Villarruel indicated no relevant financial relationships.
Hellen Jumo indicated no relevant financial relationships.
Lavender Micalo indicated no relevant financial relationships.
Laura Mcenerney indicated no relevant financial relationships.
Danny Issa: Boston Scientific – Consultant, Speakers Bureau. Eli Lilly – Speakers Bureau.
Fadi Dahoud, BS1, Elizza E. Villarruel, BS2, Hellen Jumo, BSc1, Lavender Micalo, BS1, Laura Mcenerney, MD3, Danny Issa, MD1. P3156 - Direct Visualization of Hepatocellular Carcinoma with Complete Bile Duct Invasion Using Peroral Cholangioscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
