Monday Poster Session
Category: Obesity
P3160 - Outcomes After Major Adverse Cardiovascular Events in MASLD Patients: A Nationwide Inpatient Sample Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Prince A. Ameyaw, MD
Yale New Haven Health, Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
Prince A. Ameyaw, MD1, Sarpong Boateng, MD, MPH1, Amoafo Boampong, MD2, Derek Ugwendum, MD, MPH3, Tawanda Zinyandu, MD, MPH1, Isaac Adjei Opoku, MD1, Ashraf Ahmed, MD1, Basile Njei, MD4
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Howard University Hospital, Washington, DC; 3Richmond University Medical Center, Staten Island, NY; 4Yale University School of Medicine, New Haven, CT
Introduction: Metabolic Dysfunction-Associated Steatohepatitis Liver Disease (MASLD) is a growing public health concern due to its association with obesity and increased risk of cardiovascular events. This study investigates the outcomes after major adverse cardiovascular events (MACEs) in patients with MASLD, focusing on differences between obese and non-obese MASLD patients using data from the National Inpatient Sample (NIS).
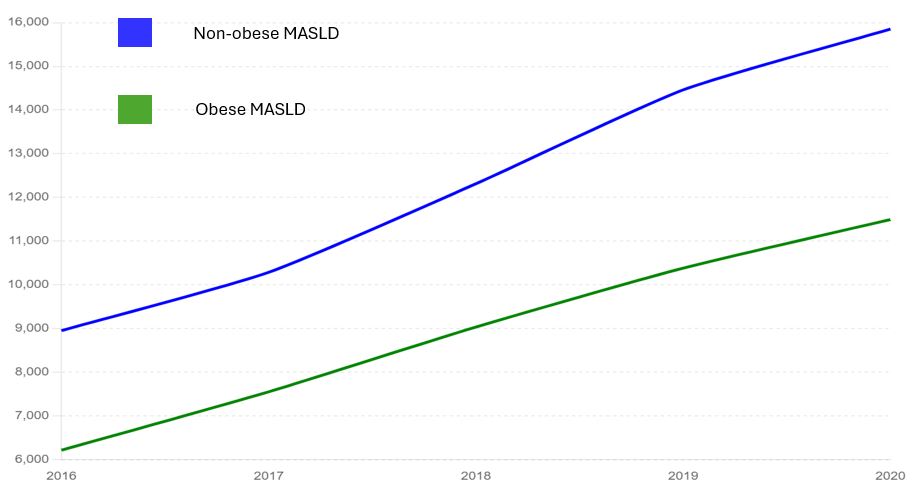
Methods: We conducted a retrospective analysis using the NIS database from 2016 to 2020, identifying patients diagnosed with MASLD who experienced MACEs. MACEs were defined as a composite of acute myocardial infarction, cardiac arrest, stroke, heart failure, and atrial fibrillation. Patient characteristics, comorbidities, and outcomes were compared between obese and non-obese MASLD patients. After adjusting for age, sex, race, smoking, cardiometabolic risk factors, hospital characteristics, socio-economic factors, prior myocardial infarction and comorbidities, multivariable logistic and Poisson regression models were used to assess the association between obesity and outcomes after MACEs in MASLD patients
Results: The study included 106,546 patients with MASLD who experienced MACEs, of which 41.9% were classified as obese. Patients with obese MASLD were younger (mean age 62.1 vs. 67.2 years, p< 0.0001) compared to non-obese MASLD patients.
Outcomes showed significant differences between the two groups. For obese MASLD patients, the adjusted odds ratio for acute kidney injury was higher (aOR: 1.080, 95% CI: 1.048–1.112, p< 0.0001) compared to non-obese MASLD patients. Obese MASLD patients also had higher adjusted odds of in-hospital death (aOR: 1.21, 95% CI: 1.14–1.28, p< 0.0001) compared to non-obese MASLD patients. Additionally, obese MASLD patients incurred higher inflation-adjusted hospital charges ($2,262.57, 95% CI: $509.27–$4,015.87, p=0.0114) and longer adjusted length of stay (aOR: 0.360, 95% CI: 0.257–0.464, p< 0.0001).
Discussion: Obesity in MASLD patients significantly influences outcomes after MACEs: obese MASLD patients are more likely to develop acute kidney injury and have higher in-hospital mortality, hospital charges, and length of stay. These findings highlight the need for tailored management strategies for obese MASLD patients to improve cardiovascular outcomes. Further research is warranted to understand the underlying mechanisms and to develop effective interventions.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Prince A. Ameyaw, MD1, Sarpong Boateng, MD, MPH1, Amoafo Boampong, MD2, Derek Ugwendum, MD, MPH3, Tawanda Zinyandu, MD, MPH1, Isaac Adjei Opoku, MD1, Ashraf Ahmed, MD1, Basile Njei, MD4. P3160 - Outcomes After Major Adverse Cardiovascular Events in MASLD Patients: A Nationwide Inpatient Sample Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Howard University Hospital, Washington, DC; 3Richmond University Medical Center, Staten Island, NY; 4Yale University School of Medicine, New Haven, CT
Introduction: Metabolic Dysfunction-Associated Steatohepatitis Liver Disease (MASLD) is a growing public health concern due to its association with obesity and increased risk of cardiovascular events. This study investigates the outcomes after major adverse cardiovascular events (MACEs) in patients with MASLD, focusing on differences between obese and non-obese MASLD patients using data from the National Inpatient Sample (NIS).
Methods: We conducted a retrospective analysis using the NIS database from 2016 to 2020, identifying patients diagnosed with MASLD who experienced MACEs. MACEs were defined as a composite of acute myocardial infarction, cardiac arrest, stroke, heart failure, and atrial fibrillation. Patient characteristics, comorbidities, and outcomes were compared between obese and non-obese MASLD patients. After adjusting for age, sex, race, smoking, cardiometabolic risk factors, hospital characteristics, socio-economic factors, prior myocardial infarction and comorbidities, multivariable logistic and Poisson regression models were used to assess the association between obesity and outcomes after MACEs in MASLD patients
Results: The study included 106,546 patients with MASLD who experienced MACEs, of which 41.9% were classified as obese. Patients with obese MASLD were younger (mean age 62.1 vs. 67.2 years, p< 0.0001) compared to non-obese MASLD patients.
Outcomes showed significant differences between the two groups. For obese MASLD patients, the adjusted odds ratio for acute kidney injury was higher (aOR: 1.080, 95% CI: 1.048–1.112, p< 0.0001) compared to non-obese MASLD patients. Obese MASLD patients also had higher adjusted odds of in-hospital death (aOR: 1.21, 95% CI: 1.14–1.28, p< 0.0001) compared to non-obese MASLD patients. Additionally, obese MASLD patients incurred higher inflation-adjusted hospital charges ($2,262.57, 95% CI: $509.27–$4,015.87, p=0.0114) and longer adjusted length of stay (aOR: 0.360, 95% CI: 0.257–0.464, p< 0.0001).
Discussion: Obesity in MASLD patients significantly influences outcomes after MACEs: obese MASLD patients are more likely to develop acute kidney injury and have higher in-hospital mortality, hospital charges, and length of stay. These findings highlight the need for tailored management strategies for obese MASLD patients to improve cardiovascular outcomes. Further research is warranted to understand the underlying mechanisms and to develop effective interventions.
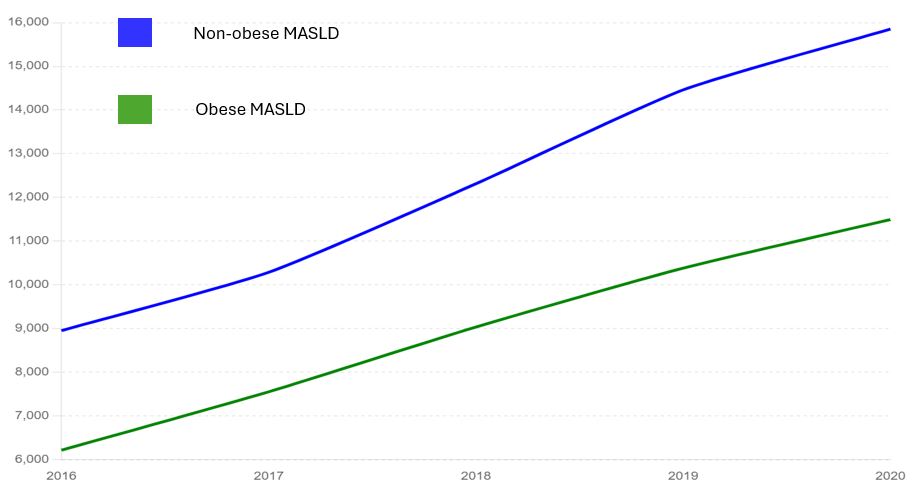
Figure: Trend of MACEs In Obese Vs Non-Obese MASLD US Hospitalizations by Year
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Prince Ameyaw indicated no relevant financial relationships.
Sarpong Boateng indicated no relevant financial relationships.
Amoafo Boampong indicated no relevant financial relationships.
Derek Ugwendum indicated no relevant financial relationships.
Tawanda Zinyandu indicated no relevant financial relationships.
Isaac Adjei Opoku indicated no relevant financial relationships.
Ashraf Ahmed indicated no relevant financial relationships.
Basile Njei indicated no relevant financial relationships.
Prince A. Ameyaw, MD1, Sarpong Boateng, MD, MPH1, Amoafo Boampong, MD2, Derek Ugwendum, MD, MPH3, Tawanda Zinyandu, MD, MPH1, Isaac Adjei Opoku, MD1, Ashraf Ahmed, MD1, Basile Njei, MD4. P3160 - Outcomes After Major Adverse Cardiovascular Events in MASLD Patients: A Nationwide Inpatient Sample Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
