Monday Poster Session
Category: Obesity
P3164 - Obesity Medication Prescribing Practices in an Urban Academic Medical Center
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sara Goff, MD
Temple University
Philadelphia, PA
Presenting Author(s)
Sara Goff, MD1, Adam C. Ehrlich, MD, MPH2, Jessica Briscoe, MD1
1Temple University, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
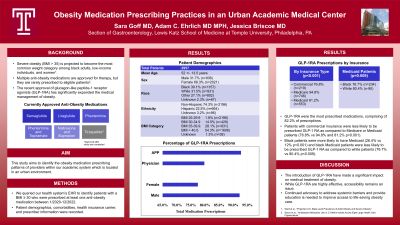
Introduction: Obesity is a highly prevalent disease with significant morbidity and mortality. Severe obesity (BMI >35) is projected to become the most common weight category among black adults, low-income individuals, and women1. Multiple anti-obesity medications (AOM) are approved for therapy, but they are rarely prescribed to eligible patients2. This study aims to identify the obesity medication prescribing patterns of providers within an academic urban health system.
Methods: Our electronic health record was queried for obese patients who were prescribed at least one AOM: semaglutide, liraglutide, phentermine alone, or with topiramate, and naltrexone/bupropion between 1/2020 to 12/2022. Patient demographics, comorbidities, health insurance carrier, and prescriber information were recorded.
Results: A total of 2957 patients were included. Patients were predominantly female, 68.3% with a mean age of 52 years; 39.1% identifying as Black and 31.5% as White, while 74.3%identified as non-Hispanic. GLP-1 receptor agonists (GLP-1 RA), semaglutide and liraglutide, were the most prescribed medications, with 82.2% of prescriptions. Males were more likely than females to be prescribed a GLP-1 RA at 92.3% compared to 77.5% (p < 0.001). Those with a BMI 30-34.9 were the most likely to receive a GLP-1 RA (84.8%) as compared to other BMI categories. Physicians were less likely to prescribe a GLP-1 RA (79.8%) as compared to APPs (92.8%). Patients with commercial insurance were less likely to be prescribed GLP-1 RA as compared to Medicare or Medicaid patients (76.8% vs 94.8% and 81.2% p< 0.001). Black patients were more likely to have Medicaid insurance (26.4% vs 12% p< 0.001 ) and Black Medicaid patients were less likely to be prescribed GLP-1 RA as compared to white patients (76.7% vs 80.4% p=0.009).
Discussion: GLP-1 RA are highly effective for the treatment of obesity, but accessibility remains an issue. Our study notes that patients at our institution with commercial insurance, Black patients as compared to White patients with Medicaid, and women were less likely to be prescribed GLP-1 RA. Continued advocacy to address systemic barriers and provider education is needed to improve access to life-saving obesity care.
1. Ward et al., “Projected U.S. State-Level Prevalence of Adult Obesity and Severe Obesity.”
2. Saxon et al., “Antiobesity Medication Use in 2.2 Million Adults Across Eight Large Health Care Organizations.”
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sara Goff, MD1, Adam C. Ehrlich, MD, MPH2, Jessica Briscoe, MD1. P3164 - Obesity Medication Prescribing Practices in an Urban Academic Medical Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Temple University, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: Obesity is a highly prevalent disease with significant morbidity and mortality. Severe obesity (BMI >35) is projected to become the most common weight category among black adults, low-income individuals, and women1. Multiple anti-obesity medications (AOM) are approved for therapy, but they are rarely prescribed to eligible patients2. This study aims to identify the obesity medication prescribing patterns of providers within an academic urban health system.
Methods: Our electronic health record was queried for obese patients who were prescribed at least one AOM: semaglutide, liraglutide, phentermine alone, or with topiramate, and naltrexone/bupropion between 1/2020 to 12/2022. Patient demographics, comorbidities, health insurance carrier, and prescriber information were recorded.
Results: A total of 2957 patients were included. Patients were predominantly female, 68.3% with a mean age of 52 years; 39.1% identifying as Black and 31.5% as White, while 74.3%identified as non-Hispanic. GLP-1 receptor agonists (GLP-1 RA), semaglutide and liraglutide, were the most prescribed medications, with 82.2% of prescriptions. Males were more likely than females to be prescribed a GLP-1 RA at 92.3% compared to 77.5% (p < 0.001). Those with a BMI 30-34.9 were the most likely to receive a GLP-1 RA (84.8%) as compared to other BMI categories. Physicians were less likely to prescribe a GLP-1 RA (79.8%) as compared to APPs (92.8%). Patients with commercial insurance were less likely to be prescribed GLP-1 RA as compared to Medicare or Medicaid patients (76.8% vs 94.8% and 81.2% p< 0.001). Black patients were more likely to have Medicaid insurance (26.4% vs 12% p< 0.001 ) and Black Medicaid patients were less likely to be prescribed GLP-1 RA as compared to white patients (76.7% vs 80.4% p=0.009).
Discussion: GLP-1 RA are highly effective for the treatment of obesity, but accessibility remains an issue. Our study notes that patients at our institution with commercial insurance, Black patients as compared to White patients with Medicaid, and women were less likely to be prescribed GLP-1 RA. Continued advocacy to address systemic barriers and provider education is needed to improve access to life-saving obesity care.
1. Ward et al., “Projected U.S. State-Level Prevalence of Adult Obesity and Severe Obesity.”
2. Saxon et al., “Antiobesity Medication Use in 2.2 Million Adults Across Eight Large Health Care Organizations.”
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sara Goff indicated no relevant financial relationships.
Adam Ehrlich: Abbvie – Consultant, Speakers Bureau. Bristol Meyers Squibb – Consultant. Eli Lilly – Consultant. Janssen – Consultant. Nestle/Aimmune – Consultant.
Jessica Briscoe indicated no relevant financial relationships.
Sara Goff, MD1, Adam C. Ehrlich, MD, MPH2, Jessica Briscoe, MD1. P3164 - Obesity Medication Prescribing Practices in an Urban Academic Medical Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
