Monday Poster Session
Category: Liver
P3095 - Patients Don’t Read Medical Textbooks: A Case Study Showing an Atypical Presentation of Liver Pathology
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Adolfo A. Torres, BS
Joan C. Edwards School of Medicine, Marshall University
Huntington, WV
Presenting Author(s)
Adolfo A. Torres, BS1, Lily Cessna, BS2, Para Dhulashia, 3, Isha Garala, 3, M'hamed Turki, MD1, Logan Lawrence, PA1, Krista L. Denning, MD1, Tejas Joshi, MD2
1Joan C. Edwards School of Medicine, Marshall University, Huntington, WV; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 3Rutgers University, Parsippany, NJ
Introduction: Primary biliary cholangitis (PBC) is an uncommon liver disease with well-defined diagnostic criteria, but certain subtypes might remain underdiagnosed. We are describing a patient with an ambiguous presentation.
Case Description/Methods: This case follows the course a 37-year-old male from West Virginia with a long history of IV drug use. The patient came to the hospital for a CT scan showing L5-S1 osteomyelitis. Labs showed high ESR (57), CRP (8.6), pancytopenia (Hb 9.3, WBC 3.99, platelets 61), and alkaline phosphatase (ALP) of 122.
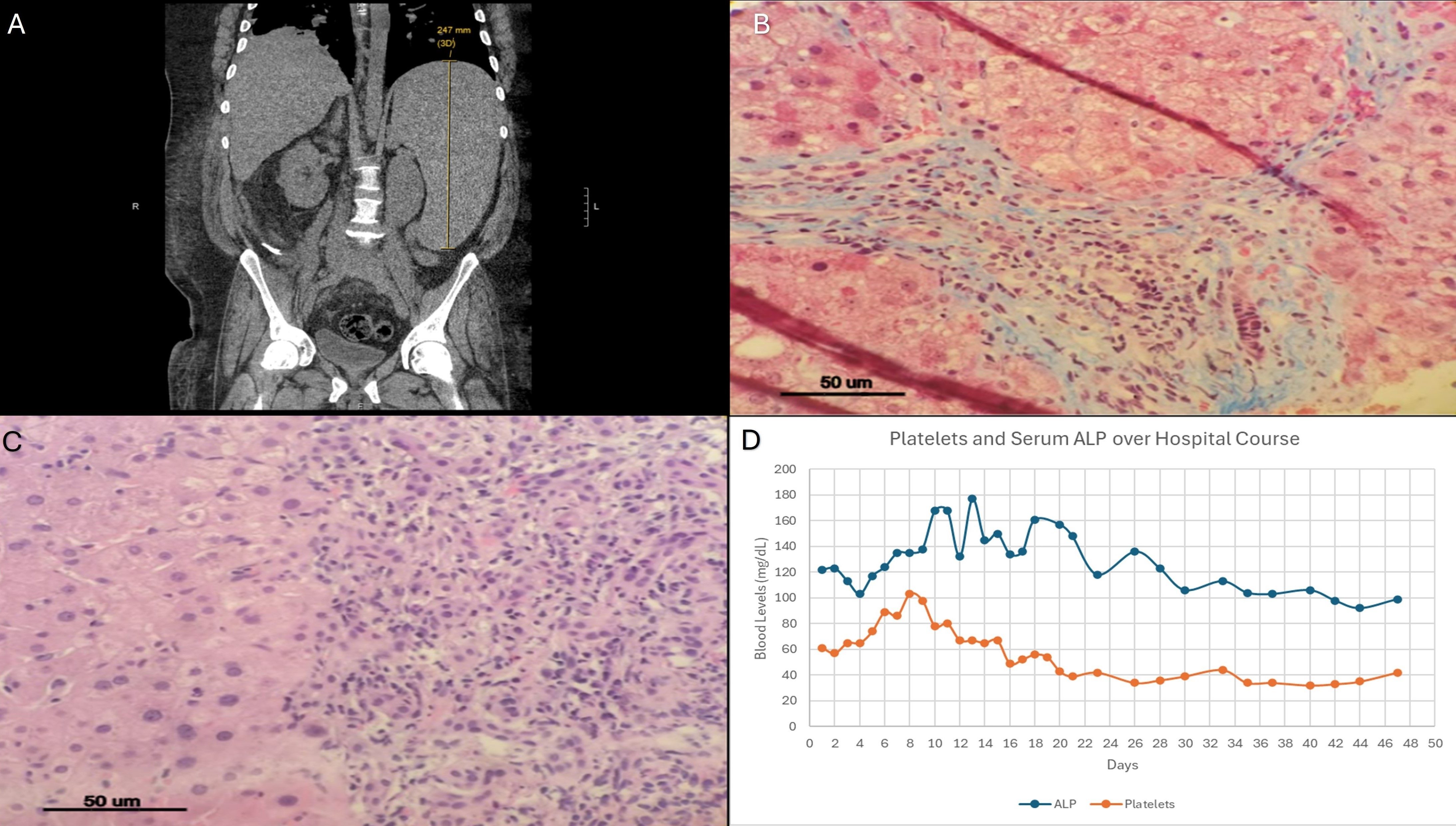
Imaging revealed marked splenomegaly (30.3cm) (fig 1(a)) and a coarse, nodular, enlarged liver (18cm). Duplex ultrasound (US) showed patent portal and hepatic circulation. Given the patient’s drug use, suspicion for viral or alcoholic etiology was high. The elevated ALP was attributed to osteomyelitis.
Viral hepatitis and HIV screening were negative. Phosphatidylethanol was negative, anti-nuclear antibody (ANA) was positive ( > 1:80), anti-mitochondrial antibody (AMA) was equivocal (22.3), anti-smooth muscle antibody was negative, ceruloplasmin was elevated (32.9), and IgM was (412).
Endoscopic US with liver biopsies revealed portal hypertension with a hepatic venous pressure gradient of 9, and bridging fibrosis, elevated collagen, and a biliary pattern of injury (fig 1(b,c)).
Despite the above social risk factors and the osseous lesion which initially attributed to the elevated ALP, we elected to initiate ursodeoxycholic acid (UDCA) on day 21 based on the biliary pattern of injury on the biopsy. ALP normalized within 4 weeks (27 days) (fig 1(d)).
The patient was discharged on day 47 and was seen in the clinic. Elastography showed F4 fibrosis (20.1 kPa) and S3 steatosis (308 dB/m). UDCA was tolerated, and he followed up regularly for monitoring. His thrombocytopenia resolved after 14 months (fig 1(d)).
Discussion: Positive AMA is pathognomonic (90-95% specificity) for PBC in the setting of isolated elevation of ALP. Its prevalence is only 40 per 100,000, and AMA negative PBC is highly uncommon. Without a positive AMA, PBC becomes a diagnosis of exclusion. Additionally, PBC is 10-fold more common in women. These factors underlie the challenging presentation of this patient combined further with multiple risk factors to explain liver disease. The initial assumption that this patient’s liver pathology was solely secondary to drug use highlights the need for all patients to receive comprehensive and unbiased care regardless of social determinants of health.
Disclosures:
Adolfo A. Torres, BS1, Lily Cessna, BS2, Para Dhulashia, 3, Isha Garala, 3, M'hamed Turki, MD1, Logan Lawrence, PA1, Krista L. Denning, MD1, Tejas Joshi, MD2. P3095 - Patients Don’t Read Medical Textbooks: A Case Study Showing an Atypical Presentation of Liver Pathology, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Joan C. Edwards School of Medicine, Marshall University, Huntington, WV; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 3Rutgers University, Parsippany, NJ
Introduction: Primary biliary cholangitis (PBC) is an uncommon liver disease with well-defined diagnostic criteria, but certain subtypes might remain underdiagnosed. We are describing a patient with an ambiguous presentation.
Case Description/Methods: This case follows the course a 37-year-old male from West Virginia with a long history of IV drug use. The patient came to the hospital for a CT scan showing L5-S1 osteomyelitis. Labs showed high ESR (57), CRP (8.6), pancytopenia (Hb 9.3, WBC 3.99, platelets 61), and alkaline phosphatase (ALP) of 122.
Imaging revealed marked splenomegaly (30.3cm) (fig 1(a)) and a coarse, nodular, enlarged liver (18cm). Duplex ultrasound (US) showed patent portal and hepatic circulation. Given the patient’s drug use, suspicion for viral or alcoholic etiology was high. The elevated ALP was attributed to osteomyelitis.
Viral hepatitis and HIV screening were negative. Phosphatidylethanol was negative, anti-nuclear antibody (ANA) was positive ( > 1:80), anti-mitochondrial antibody (AMA) was equivocal (22.3), anti-smooth muscle antibody was negative, ceruloplasmin was elevated (32.9), and IgM was (412).
Endoscopic US with liver biopsies revealed portal hypertension with a hepatic venous pressure gradient of 9, and bridging fibrosis, elevated collagen, and a biliary pattern of injury (fig 1(b,c)).
Despite the above social risk factors and the osseous lesion which initially attributed to the elevated ALP, we elected to initiate ursodeoxycholic acid (UDCA) on day 21 based on the biliary pattern of injury on the biopsy. ALP normalized within 4 weeks (27 days) (fig 1(d)).
The patient was discharged on day 47 and was seen in the clinic. Elastography showed F4 fibrosis (20.1 kPa) and S3 steatosis (308 dB/m). UDCA was tolerated, and he followed up regularly for monitoring. His thrombocytopenia resolved after 14 months (fig 1(d)).
Discussion: Positive AMA is pathognomonic (90-95% specificity) for PBC in the setting of isolated elevation of ALP. Its prevalence is only 40 per 100,000, and AMA negative PBC is highly uncommon. Without a positive AMA, PBC becomes a diagnosis of exclusion. Additionally, PBC is 10-fold more common in women. These factors underlie the challenging presentation of this patient combined further with multiple risk factors to explain liver disease. The initial assumption that this patient’s liver pathology was solely secondary to drug use highlights the need for all patients to receive comprehensive and unbiased care regardless of social determinants of health.
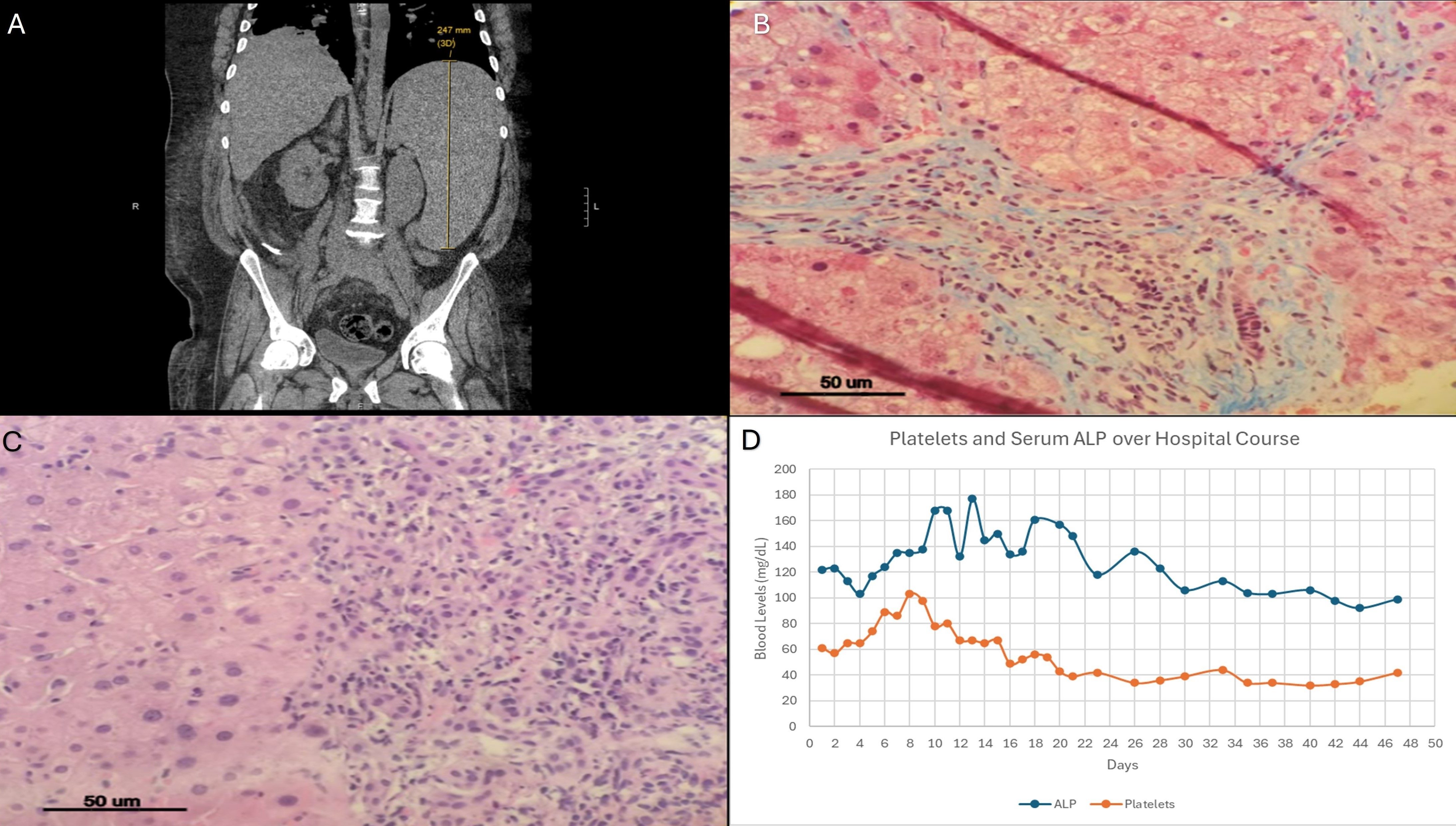
Figure: Fig. 1 | CT imaging, liver biopsies, and progression of platelet and ALP levels; (a) Coronal view of the patient's non-contrast CT of the spine and lumbar region that incidentally discovered massive splenomegaly. The spleen can be seen measuring 24.7 cm in this cross-section; (b) Liver needle core biopsy at 400x magnification with trichrome staining; (c) Liver needle core biopsy at 400x magnification with hematoxylin and eosin staining; (d) Scatter plot showing the progression of the patient's platelet levels and ALP levels throughout his hospital stay.
Disclosures:
Adolfo Torres indicated no relevant financial relationships.
Lily Cessna indicated no relevant financial relationships.
Para Dhulashia indicated no relevant financial relationships.
Isha Garala indicated no relevant financial relationships.
M'hamed Turki indicated no relevant financial relationships.
Logan Lawrence indicated no relevant financial relationships.
Krista Denning indicated no relevant financial relationships.
Tejas Joshi: Cook – Consultant. Echosens – Consultant. Gilead – Key Opinion Leader.
Adolfo A. Torres, BS1, Lily Cessna, BS2, Para Dhulashia, 3, Isha Garala, 3, M'hamed Turki, MD1, Logan Lawrence, PA1, Krista L. Denning, MD1, Tejas Joshi, MD2. P3095 - Patients Don’t Read Medical Textbooks: A Case Study Showing an Atypical Presentation of Liver Pathology, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
