Monday Poster Session
Category: Liver
P3096 - Esophageal and Gastric Variceal Hemorrhage Lead to Discovery of Isolated Hepatic Decompensation Secondary to A1AT Deficiency
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Adolfo A. Torres, BS
Joan C. Edwards School of Medicine, Marshall University
Huntington, WV
Presenting Author(s)
Adolfo A. Torres, BS1, Lily Cessna, BS2, Para Dhulashia, 3, Isha Garala, 3, M'hamed Turki, MD1, Tejas Joshi, MD2
1Joan C. Edwards School of Medicine, Marshall University, Huntington, WV; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 3Rutgers University, Parsippany, NJ
Introduction: Alpha-1-antitrypsin deficiency (AATD) is an autosomal codominant heritable cause of early-onset emphysema and cirrhosis. The ZZ phenotype is the most common manifestation of AATD and results in the toxic accumulation of abnormal alpha-1-antitrypsin (α1-AT) in the liver – leading to damage and cirrhosis.
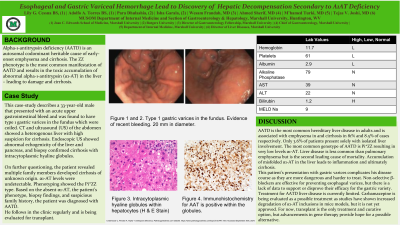
Case Description/Methods: This case-study describes a 33-year-old male that presented with an acute upper gastrointestinal bleed and was found to have type 1 gastric varices in the fundus which were coiled. CT and ultrasound (US) of the abdomen showed a heterogenous liver with high suspicion for cirrhosis. Labs were as follows: Hb 11.7, platelets 61, albumin 2.9, alkaline phosphatase (ALP) 29, AST 39, ALT 79, bilirubin 1.2. Endoscopic US showed abnormal echogenicity of the liver and pancreas, and biopsy confirmed cirrhosis with intracytoplasmic hyaline globules.
On further questioning, the patient revealed multiple family members developed cirrhosis of unknown origin. α1-AT levels were undetectable. Phenotyping showed the Pi*ZZ type. Based on the absent α1-AT, the patient’s phenotype, biopsy findings, and suspicious family history, the patient was diagnosed with AATD.
He follows in the clinic regularly and is being evaluated for transplant.
Discussion: AATD is the most common hereditary liver disease in adults and is associated with emphysema in and cirrhosis in 81% and 8.5% of cases respectively. Only 3.6% of patients present solely with isolated liver involvement. The most common genotype of AATD is Pi*ZZ resulting in very low levels α1-AT. Liver disease is less common than pulmonary emphysema but is the second leading cause of mortality. Accumulation of misfolded α1-AT in the liver leads to inflammation and ultimately cirrhosis.
This patient’s presentation with gastric varices complicates his disease course as they are more dangerous and harder to treat. Non-selective β-blockers are effective for preventing esophageal varices, but there is a lack of data to support or disprove their efficacy for the gastric variety.
Treatment for AATD liver disease is currently limited. Carbamazepine is being evaluated as a possible treatment as studies have shown increased degradation of α1-AT inclusions in mice models, but it is not yet approved. For now, transplant is the only treatment and curative option, but advancements in gene therapy provide hope for a possible alternative.
Disclosures:
Adolfo A. Torres, BS1, Lily Cessna, BS2, Para Dhulashia, 3, Isha Garala, 3, M'hamed Turki, MD1, Tejas Joshi, MD2. P3096 - Esophageal and Gastric Variceal Hemorrhage Lead to Discovery of Isolated Hepatic Decompensation Secondary to A1AT Deficiency, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Joan C. Edwards School of Medicine, Marshall University, Huntington, WV; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 3Rutgers University, Parsippany, NJ
Introduction: Alpha-1-antitrypsin deficiency (AATD) is an autosomal codominant heritable cause of early-onset emphysema and cirrhosis. The ZZ phenotype is the most common manifestation of AATD and results in the toxic accumulation of abnormal alpha-1-antitrypsin (α1-AT) in the liver – leading to damage and cirrhosis.
Case Description/Methods: This case-study describes a 33-year-old male that presented with an acute upper gastrointestinal bleed and was found to have type 1 gastric varices in the fundus which were coiled. CT and ultrasound (US) of the abdomen showed a heterogenous liver with high suspicion for cirrhosis. Labs were as follows: Hb 11.7, platelets 61, albumin 2.9, alkaline phosphatase (ALP) 29, AST 39, ALT 79, bilirubin 1.2. Endoscopic US showed abnormal echogenicity of the liver and pancreas, and biopsy confirmed cirrhosis with intracytoplasmic hyaline globules.
On further questioning, the patient revealed multiple family members developed cirrhosis of unknown origin. α1-AT levels were undetectable. Phenotyping showed the Pi*ZZ type. Based on the absent α1-AT, the patient’s phenotype, biopsy findings, and suspicious family history, the patient was diagnosed with AATD.
He follows in the clinic regularly and is being evaluated for transplant.
Discussion: AATD is the most common hereditary liver disease in adults and is associated with emphysema in and cirrhosis in 81% and 8.5% of cases respectively. Only 3.6% of patients present solely with isolated liver involvement. The most common genotype of AATD is Pi*ZZ resulting in very low levels α1-AT. Liver disease is less common than pulmonary emphysema but is the second leading cause of mortality. Accumulation of misfolded α1-AT in the liver leads to inflammation and ultimately cirrhosis.
This patient’s presentation with gastric varices complicates his disease course as they are more dangerous and harder to treat. Non-selective β-blockers are effective for preventing esophageal varices, but there is a lack of data to support or disprove their efficacy for the gastric variety.
Treatment for AATD liver disease is currently limited. Carbamazepine is being evaluated as a possible treatment as studies have shown increased degradation of α1-AT inclusions in mice models, but it is not yet approved. For now, transplant is the only treatment and curative option, but advancements in gene therapy provide hope for a possible alternative.
Disclosures:
Adolfo Torres indicated no relevant financial relationships.
Lily Cessna indicated no relevant financial relationships.
Para Dhulashia indicated no relevant financial relationships.
Isha Garala indicated no relevant financial relationships.
M'hamed Turki indicated no relevant financial relationships.
Tejas Joshi: Cook – Consultant. Echosens – Consultant. Gilead – Key Opinion Leader.
Adolfo A. Torres, BS1, Lily Cessna, BS2, Para Dhulashia, 3, Isha Garala, 3, M'hamed Turki, MD1, Tejas Joshi, MD2. P3096 - Esophageal and Gastric Variceal Hemorrhage Lead to Discovery of Isolated Hepatic Decompensation Secondary to A1AT Deficiency, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
