Monday Poster Session
Category: Liver
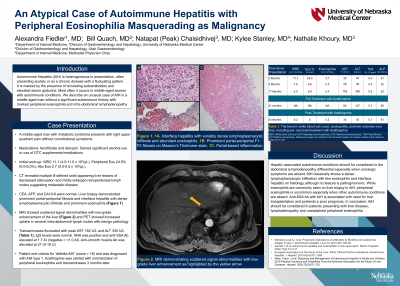
P3100 - An Atypical Case of Autoimmune Hepatitis With Peripheral Eosinophilia Masquerading as Malignancy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Alexandra Fiedler, MD
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Alexandra Fiedler, MD1, Bill Quach, MD1, Natapat Chaisidhivej, MD1, Nathalie Khoury, MD1, Kylee V. Stanley, MD2
1University of Nebraska Medical Center, Omaha, NE; 2Methodist Health System, Fremont, NE
Introduction: Autoimmune hepatitis (AIH) presents heterogeneously with the usual illness script describing a middle-aged woman with autoimmune disease developing abnormal fluctuating transaminases. We describe an uncommon AIH case with marked peripheral eosinophilia and intra-abdominal lymphadenopathy.
Case Description/Methods: A middle-aged man with metabolic syndrome presents with right upper quadrant abdominal pain without constitutional symptoms. His medications are fenofibrate and lisinopril; he denies supplements, over-the-counter medications, or significant alcohol consumption. CT abdomen with contrast reveals multiple ill-defined solid-appearing liver lesions and enlarged retroperitoneal lymph nodes (LN) suggesting metastatic disease. Labs show a white blood cell count of 11.1 x 103/µL, an absolute eosinophil count of 2700 µL with normal liver enzymes and tumor markers. Liver biopsy demonstrates prominent portal-periportal fibrosis (F2-F3) and interface hepatitis with dense lymphoplasmacytic and prominent eosinophils. MRI shows scattered signal abnormalities with low-grade enhancement of the liver. PET scan shows increased uptake in several intra-abdominal LNs without significant pathology on biopsy.
Transaminases fluctuated over the next two years with peak AST 182 U/L and ALT 335 U/L (Table 1). Total bilirubin, alkaline phosphatase, and serum IgG levels were normal. ANA was positive with elevated anti-Sjögren's-syndrome-related antigen A Ab (anti-SSA Ab) of 1.7 (Negative = < 1.0 AI). Anti-smooth muscle Ab was elevated at 27 (0-19 U). Based on the revised diagnostic scoring system for AIH, the patient met the criteria for ‘definite AIH’ (score = 16) and was diagnosed with AIH type 1. Azathioprine (AZA) was started with normalization of peripheral eosinophilia and transaminases 3 months later.
Discussion: Hepatic associated autoimmune conditions should be considered in the abdominal lymphadenopathy differential especially when oncologic symptoms are absent. AIH classically shows a dense lymphoplasmacytic infiltration with few eosinophils and interface hepatitis on histology although no feature is pathognomonic. While eosinophils are commonly seen on liver biopsy in AIH, peripheral eosinophilia is uncommon especially when other autoimmune conditions are absent. Anti-SSA Ab with AIH is associated with a need for liver transplantation and portends a poor prognosis. In conclusion, AIH should be considered in patients presenting with liver disease, lymphadenopathy and unexplained peripheral eosinophilia.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alexandra Fiedler, MD1, Bill Quach, MD1, Natapat Chaisidhivej, MD1, Nathalie Khoury, MD1, Kylee V. Stanley, MD2. P3100 - An Atypical Case of Autoimmune Hepatitis With Peripheral Eosinophilia Masquerading as Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Nebraska Medical Center, Omaha, NE; 2Methodist Health System, Fremont, NE
Introduction: Autoimmune hepatitis (AIH) presents heterogeneously with the usual illness script describing a middle-aged woman with autoimmune disease developing abnormal fluctuating transaminases. We describe an uncommon AIH case with marked peripheral eosinophilia and intra-abdominal lymphadenopathy.
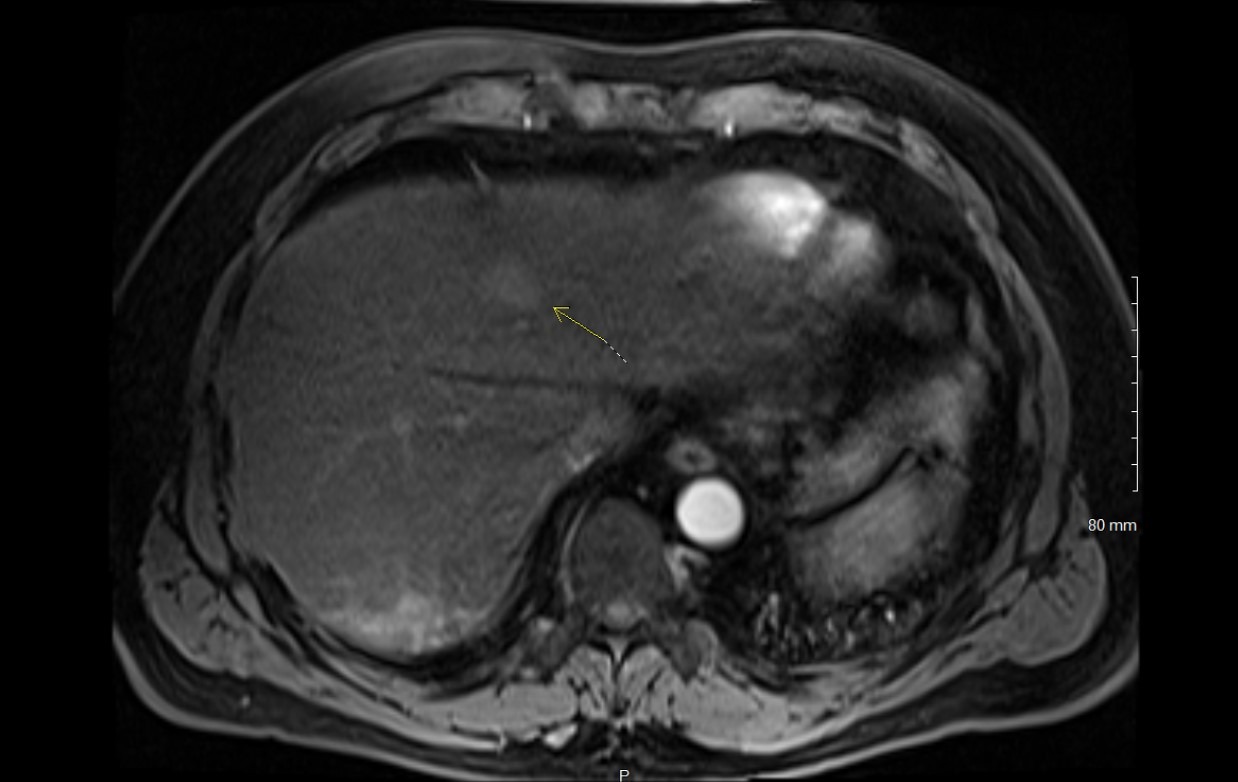
Case Description/Methods: A middle-aged man with metabolic syndrome presents with right upper quadrant abdominal pain without constitutional symptoms. His medications are fenofibrate and lisinopril; he denies supplements, over-the-counter medications, or significant alcohol consumption. CT abdomen with contrast reveals multiple ill-defined solid-appearing liver lesions and enlarged retroperitoneal lymph nodes (LN) suggesting metastatic disease. Labs show a white blood cell count of 11.1 x 103/µL, an absolute eosinophil count of 2700 µL with normal liver enzymes and tumor markers. Liver biopsy demonstrates prominent portal-periportal fibrosis (F2-F3) and interface hepatitis with dense lymphoplasmacytic and prominent eosinophils. MRI shows scattered signal abnormalities with low-grade enhancement of the liver. PET scan shows increased uptake in several intra-abdominal LNs without significant pathology on biopsy.
Transaminases fluctuated over the next two years with peak AST 182 U/L and ALT 335 U/L (Table 1). Total bilirubin, alkaline phosphatase, and serum IgG levels were normal. ANA was positive with elevated anti-Sjögren's-syndrome-related antigen A Ab (anti-SSA Ab) of 1.7 (Negative = < 1.0 AI). Anti-smooth muscle Ab was elevated at 27 (0-19 U). Based on the revised diagnostic scoring system for AIH, the patient met the criteria for ‘definite AIH’ (score = 16) and was diagnosed with AIH type 1. Azathioprine (AZA) was started with normalization of peripheral eosinophilia and transaminases 3 months later.
Discussion: Hepatic associated autoimmune conditions should be considered in the abdominal lymphadenopathy differential especially when oncologic symptoms are absent. AIH classically shows a dense lymphoplasmacytic infiltration with few eosinophils and interface hepatitis on histology although no feature is pathognomonic. While eosinophils are commonly seen on liver biopsy in AIH, peripheral eosinophilia is uncommon especially when other autoimmune conditions are absent. Anti-SSA Ab with AIH is associated with a need for liver transplantation and portends a poor prognosis. In conclusion, AIH should be considered in patients presenting with liver disease, lymphadenopathy and unexplained peripheral eosinophilia.
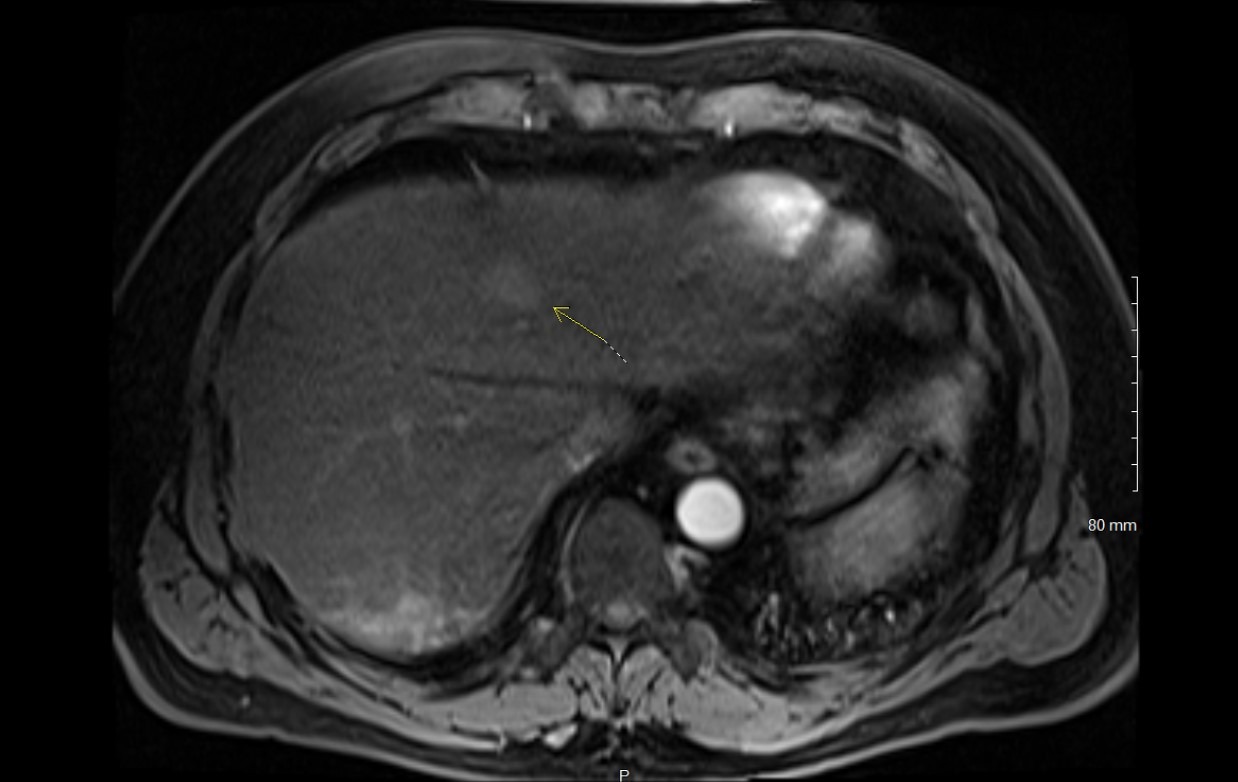
Figure: Figure 1: MRI demonstrating scattered signal abnormalities with low-grade enhancement of the liver as highlighted by the yellow arrow.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alexandra Fiedler indicated no relevant financial relationships.
Bill Quach indicated no relevant financial relationships.
Natapat Chaisidhivej indicated no relevant financial relationships.
Nathalie Khoury indicated no relevant financial relationships.
Kylee Stanley indicated no relevant financial relationships.
Alexandra Fiedler, MD1, Bill Quach, MD1, Natapat Chaisidhivej, MD1, Nathalie Khoury, MD1, Kylee V. Stanley, MD2. P3100 - An Atypical Case of Autoimmune Hepatitis With Peripheral Eosinophilia Masquerading as Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
