Monday Poster Session
Category: Liver
P3015 - Crossing Boundaries: Navigating the Diagnostic Labyrinth of Hepatic and Pulmonary Actinomycosis Post-COVID
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Dimo Dimitrov, MD
St. Elizabeth's Medical Center, Boston University School of Medicine
Boston, MA
Presenting Author(s)
Dimo Dimitrov, MD, Jad Mitri, MD, Hind El Naamani, MD, Claudia Nader, MD
St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA
Introduction: Actinomycosis, primarily caused by Actinomyces israelii, presents significant diagnostic challenges due to its varied clinical manifestations, rarity, and slow progression. It characteristically penetrates mucosal barriers, spreads across anatomical planes and mimics malignancies. While commonly affecting the cervicofacial area, it can also occur in the thorax and abdomen, with simultaneous hepatic and lung actinomycosis being particularly rare.
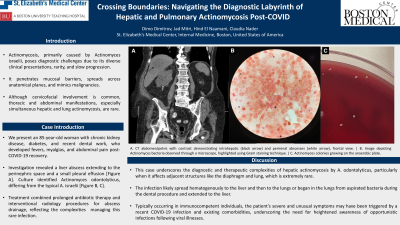
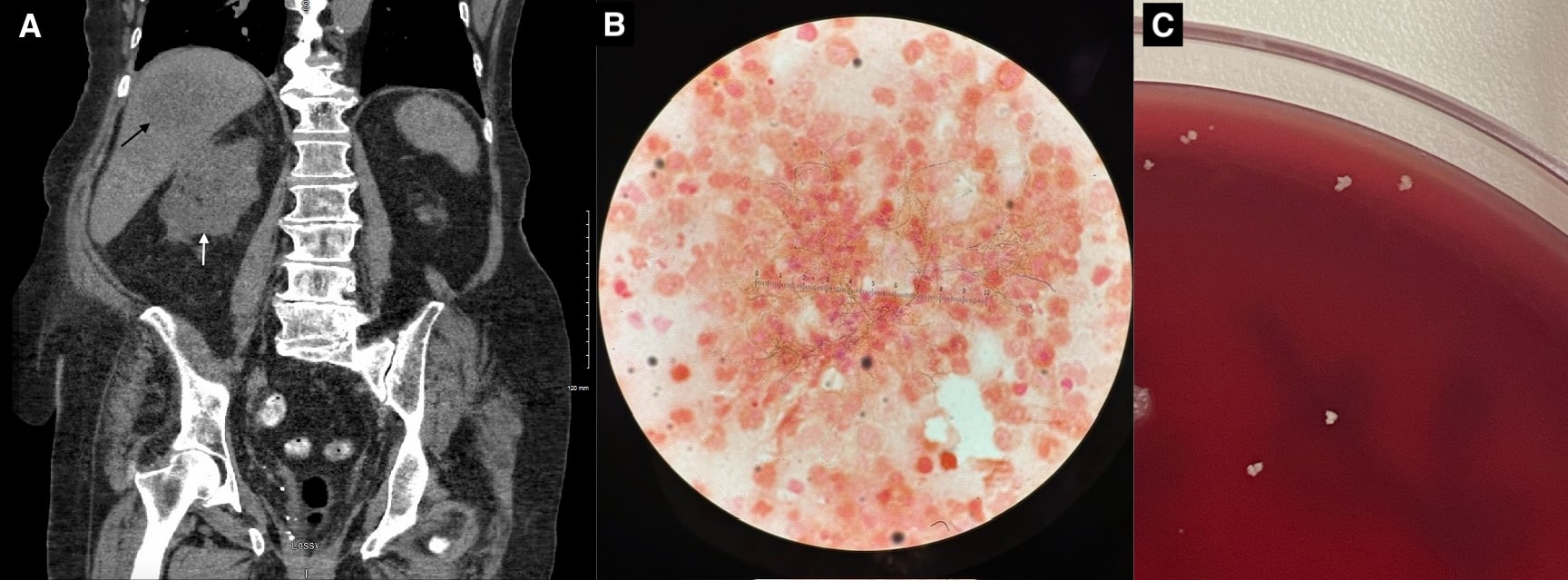
Case Description/Methods: We report a unique case of an 85-year-old woman with chronic kidney disease, diabetes, hypertension, and recent dental work, who developed fevers, myalgias, and abdominal pain weeks after recovering from COVID-19. Workup revealed a liver abscess, extending to the right perinephric space and a small pleural effusion. Gram stain of abscess aspirate showed gram-positive, branching filamentous rods, negative on modified AFB stain. Cultures grew Actinomyces odontolyticus, differing from the more common A. israelii. The hospital stay was complicated by acute hypoxic respiratory failure with CT evidence of an expanded, loculated right-sided pleural effusion. Treatment combined prolonged antibiotic therapy with ampicillin/sulbactam and interventional radiology procedures for abscess drainage, reflecting the complexities of managing this rare infection. Due to her refractory loculated pleural effusion, the patient was considered but deemed unsuitable for video-assisted thoracoscopic surgery and discharged on a prolonged antibiotic regimen.
Discussion: This case illustrates the diagnostic and therapeutic challenges of hepatic actinomycosis caused by A. odontolyticus, particularly when it affects adjacent structures like the diaphragm and lung, which is extremely rare. The infection likely spread hematogenously to the liver and then to the lungs or began in the lungs from aspirated bacteria during the dental procedure and extended to the liver. Typically occurring in immunocompetent individuals, the patient's severe presentation might have been triggered by a recent COVID-19 infection and existing comorbidities, underscoring the need for heightened awareness of atypical presentations of infections following viral illnesses. This case emphasizes the need to consider Actinomyces as the culprit organism in hepatic abscesses and supports using long-term antibiotics and drainage. It also highlights the need for more research into opportunistic bacterial infections following COVID-19-related immune dysregulation.
Disclosures:
Dimo Dimitrov, MD, Jad Mitri, MD, Hind El Naamani, MD, Claudia Nader, MD. P3015 - Crossing Boundaries: Navigating the Diagnostic Labyrinth of Hepatic and Pulmonary Actinomycosis Post-COVID, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA
Introduction: Actinomycosis, primarily caused by Actinomyces israelii, presents significant diagnostic challenges due to its varied clinical manifestations, rarity, and slow progression. It characteristically penetrates mucosal barriers, spreads across anatomical planes and mimics malignancies. While commonly affecting the cervicofacial area, it can also occur in the thorax and abdomen, with simultaneous hepatic and lung actinomycosis being particularly rare.
Case Description/Methods: We report a unique case of an 85-year-old woman with chronic kidney disease, diabetes, hypertension, and recent dental work, who developed fevers, myalgias, and abdominal pain weeks after recovering from COVID-19. Workup revealed a liver abscess, extending to the right perinephric space and a small pleural effusion. Gram stain of abscess aspirate showed gram-positive, branching filamentous rods, negative on modified AFB stain. Cultures grew Actinomyces odontolyticus, differing from the more common A. israelii. The hospital stay was complicated by acute hypoxic respiratory failure with CT evidence of an expanded, loculated right-sided pleural effusion. Treatment combined prolonged antibiotic therapy with ampicillin/sulbactam and interventional radiology procedures for abscess drainage, reflecting the complexities of managing this rare infection. Due to her refractory loculated pleural effusion, the patient was considered but deemed unsuitable for video-assisted thoracoscopic surgery and discharged on a prolonged antibiotic regimen.
Discussion: This case illustrates the diagnostic and therapeutic challenges of hepatic actinomycosis caused by A. odontolyticus, particularly when it affects adjacent structures like the diaphragm and lung, which is extremely rare. The infection likely spread hematogenously to the liver and then to the lungs or began in the lungs from aspirated bacteria during the dental procedure and extended to the liver. Typically occurring in immunocompetent individuals, the patient's severe presentation might have been triggered by a recent COVID-19 infection and existing comorbidities, underscoring the need for heightened awareness of atypical presentations of infections following viral illnesses. This case emphasizes the need to consider Actinomyces as the culprit organism in hepatic abscesses and supports using long-term antibiotics and drainage. It also highlights the need for more research into opportunistic bacterial infections following COVID-19-related immune dysregulation.
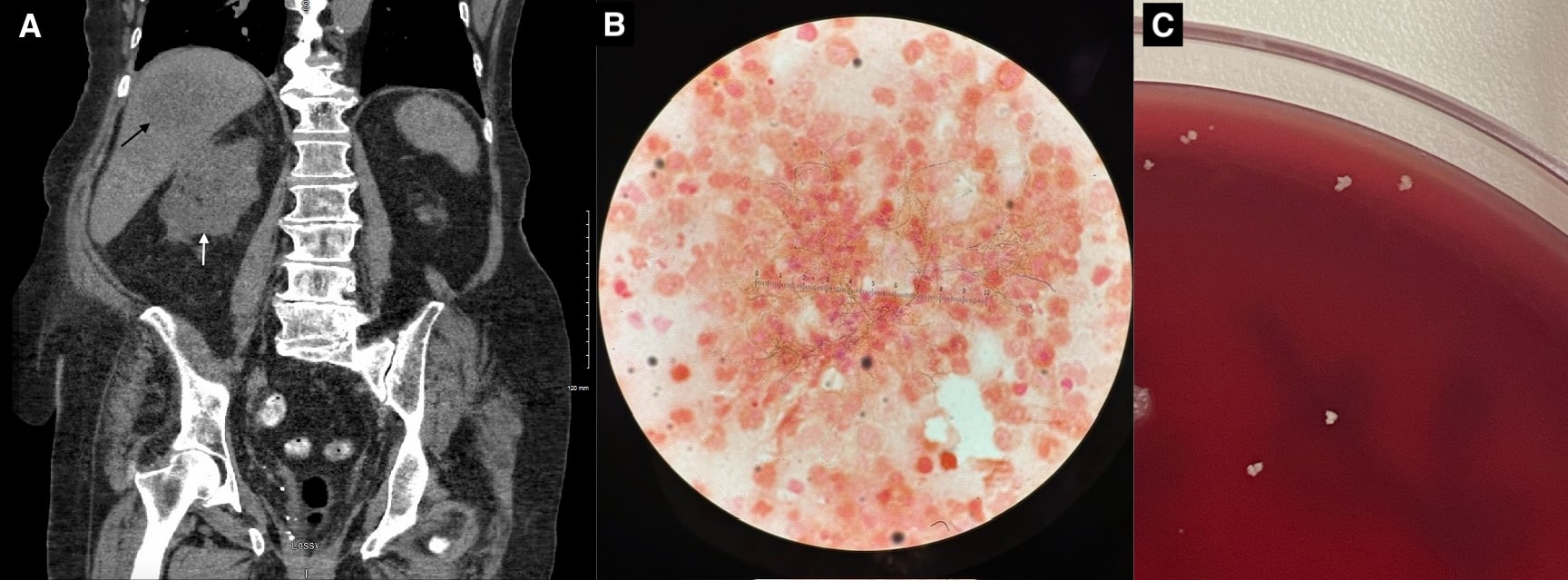
Figure: A. CT abdomen/pelvis with contrast demonstrating intrahepatic (black arrow) and perirenal abscesses (white arrow), frontal view. | B. Image depicting Actinomyces bacteria observed through a microscope, highlighted using Gram staining technique. | C. Actinomyces colonies growing on the anaerobic plate.
Disclosures:
Dimo Dimitrov indicated no relevant financial relationships.
Jad Mitri indicated no relevant financial relationships.
Hind El Naamani indicated no relevant financial relationships.
Claudia Nader indicated no relevant financial relationships.
Dimo Dimitrov, MD, Jad Mitri, MD, Hind El Naamani, MD, Claudia Nader, MD. P3015 - Crossing Boundaries: Navigating the Diagnostic Labyrinth of Hepatic and Pulmonary Actinomycosis Post-COVID, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
