Monday Poster Session
Category: Liver
P2937 - Clinical Features of Alcohol-Related Hepatitis and Mortality Trends in the Pre- and Post-COVID Era
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Regis Lee, DO
HCA Riverside Community Hospital
Riverside, CA
Presenting Author(s)
Regis Lee, DO1, Oluwaposi Omiwade, MD2, Julio A. Gutierrez, MD3, Joseph J. Alukal, MD4
1HCA Riverside Community Hospital, Riverside, CA; 2Scripps Mercy Hospital, San Diego, CA; 3Scripps Clinic, San Diego, CA; 4University of California Riverside, Riverside, CA
Introduction: Alcoholic-associated hepatitis (AH) is a severe form of alcohol-related liver disease (ALD) characterized by jaundice and liver failure with a 30-day mortality between 15-40% based on the severity. The objective of our study was to identify clinical features of patients hospitalized with AH in the United States and determine trends in mortality in the post-COVID era in comparison to the pre-COVID era.
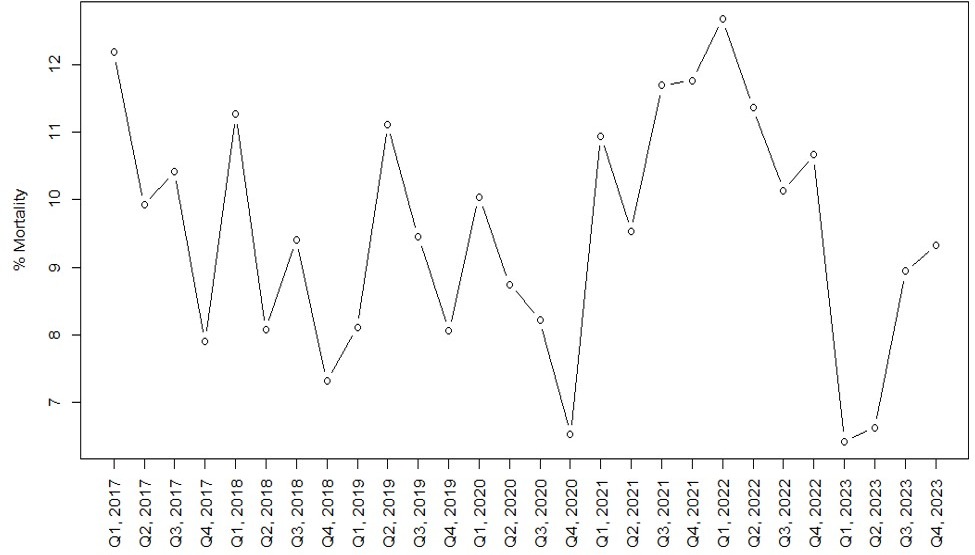
Methods: This retrospective study from 1/2017 to 12/2023 involved 186 HCA Healthcare hospitals throughout the US where de-identified electronic health data was used to identify patients admitted with AH. The HCA Healthcare system is a large network consisting of community hospitals spread across 19 states. AH was diagnosed using a combination of ICD-10 codes and biochemical parameters (total bilirubin ≥ 3 mg/dL on admission, AST 50-400 IU/L and AST/ALT > 1.5). We divided the time period into 3 eras: pre-COVID (2017-19), COVID (2020-21) and post-COVID (2022-23). Each year was further subdivided into 4 quarters and we analyzed 28 different time points to assess trends in mortality.
Results: During this study period, we identified 10,864 patients hospitalized for AH. They had an average age of 49 years and were majority Male (63%) and Caucasian (66%), with a median bilirubin of 9 mg/dL, MELD score of 22, and Maddrey Discriminant Function (MDF) of 38. The most frequent complication in our cohort was ascites (70%), followed by infections (25%), gastrointestinal (GI) bleeding (21%), and hepatic encephalopathy (6%). We also found that 4% of patients with AH experienced respiratory failure requiring intubation and 2% required dialysis. The overall in-hospital mortality in our cohort during this time period was 9.6%. The Cochran Armitage test for mortality trends between the 3 eras was not significant, indicating no linear trend to the data (p = 0.817). Patients who died had a higher MELD score (29 vs 21) and MDF (65 vs 36) compared to those who survived hospital stay. These patients were sicker than their counterparts and had more complications leading to mortality as shown in Table 1.
Discussion: Our study shows that complications of portal hypertension such as ascites are common in those hospitalized with AH and can lead to significant morbidity and mortality. Data from prior studies have revealed that admissions for AH have risen during the pandemic, however our study shows that mortality rates for AH in the pandemic and post-pandemic era have remained similar to the pre-pandemic time period.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Regis Lee, DO1, Oluwaposi Omiwade, MD2, Julio A. Gutierrez, MD3, Joseph J. Alukal, MD4. P2937 - Clinical Features of Alcohol-Related Hepatitis and Mortality Trends in the Pre- and Post-COVID Era, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HCA Riverside Community Hospital, Riverside, CA; 2Scripps Mercy Hospital, San Diego, CA; 3Scripps Clinic, San Diego, CA; 4University of California Riverside, Riverside, CA
Introduction: Alcoholic-associated hepatitis (AH) is a severe form of alcohol-related liver disease (ALD) characterized by jaundice and liver failure with a 30-day mortality between 15-40% based on the severity. The objective of our study was to identify clinical features of patients hospitalized with AH in the United States and determine trends in mortality in the post-COVID era in comparison to the pre-COVID era.
Methods: This retrospective study from 1/2017 to 12/2023 involved 186 HCA Healthcare hospitals throughout the US where de-identified electronic health data was used to identify patients admitted with AH. The HCA Healthcare system is a large network consisting of community hospitals spread across 19 states. AH was diagnosed using a combination of ICD-10 codes and biochemical parameters (total bilirubin ≥ 3 mg/dL on admission, AST 50-400 IU/L and AST/ALT > 1.5). We divided the time period into 3 eras: pre-COVID (2017-19), COVID (2020-21) and post-COVID (2022-23). Each year was further subdivided into 4 quarters and we analyzed 28 different time points to assess trends in mortality.
Results: During this study period, we identified 10,864 patients hospitalized for AH. They had an average age of 49 years and were majority Male (63%) and Caucasian (66%), with a median bilirubin of 9 mg/dL, MELD score of 22, and Maddrey Discriminant Function (MDF) of 38. The most frequent complication in our cohort was ascites (70%), followed by infections (25%), gastrointestinal (GI) bleeding (21%), and hepatic encephalopathy (6%). We also found that 4% of patients with AH experienced respiratory failure requiring intubation and 2% required dialysis. The overall in-hospital mortality in our cohort during this time period was 9.6%. The Cochran Armitage test for mortality trends between the 3 eras was not significant, indicating no linear trend to the data (p = 0.817). Patients who died had a higher MELD score (29 vs 21) and MDF (65 vs 36) compared to those who survived hospital stay. These patients were sicker than their counterparts and had more complications leading to mortality as shown in Table 1.
Discussion: Our study shows that complications of portal hypertension such as ascites are common in those hospitalized with AH and can lead to significant morbidity and mortality. Data from prior studies have revealed that admissions for AH have risen during the pandemic, however our study shows that mortality rates for AH in the pandemic and post-pandemic era have remained similar to the pre-pandemic time period.
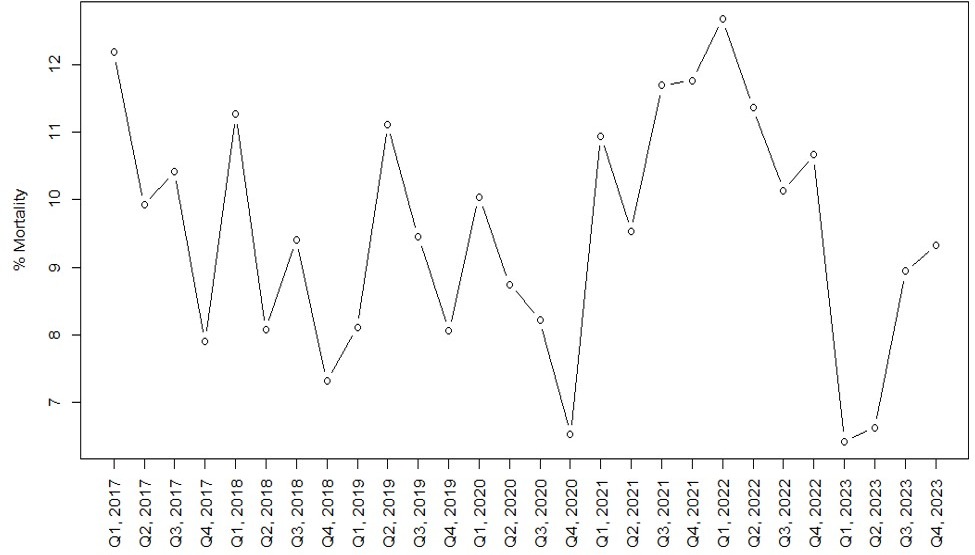
Figure: Figure 1: Percentage of mortalities in AH admissions over time
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Regis Lee indicated no relevant financial relationships.
Oluwaposi Omiwade indicated no relevant financial relationships.
Julio Gutierrez indicated no relevant financial relationships.
Joseph Alukal indicated no relevant financial relationships.
Regis Lee, DO1, Oluwaposi Omiwade, MD2, Julio A. Gutierrez, MD3, Joseph J. Alukal, MD4. P2937 - Clinical Features of Alcohol-Related Hepatitis and Mortality Trends in the Pre- and Post-COVID Era, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
