Monday Poster Session
Category: Liver
P2944 - The Burden of Liver Cancer in Sub-Saharan Africa: An Analysis From the Global Burden of Disease Database
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- OA
Omar Al Ta'ani, MD
Allegheny Health Network
Pittsburgh, PA
Presenting Author(s)
Omar Al Ta'ani, MD1, Yazan Al-Ajlouni, MD2, Yahya Alhalalmeh, MD3, Sharifeh Almasaid, MD4, Taimur S. Muzammil, MD5, Tyrell Daniel, MD5, Basile Njei, MD6
1Allegheny Health Network, Pittsburgh, PA; 2Staten Island University Hospital, Northwell Health, New York, NY; 3New York Medical College - Saint Michael's Medical Center, Newark, NJ; 4SUNY Upstate Medical University, Johnson City, TN; 5Allegheny General Hospital, Pittsburgh, PA; 6Yale University School of Medicine, New Haven, CT
Introduction: Liver cancer poses a significant health burden in Sub-Saharan Africa (SSA), with some of the highest incidence and mortality rates globally. The region's high prevalence of hepatitis B and C, along with aflatoxin exposure and limited healthcare infrastructure, exacerbates the problem. Our study analyzes trends in liver cancer incidence, Disability-Adjusted Life Years (DALYs), and mortality in SSA from 1990 to 2021, providing insights to inform targeted interventions and policy decisions.
Methods: Data from the Global Burden of Disease (GBD) dataset were used to analyze the burden of liver cancer from 1990 to 2021. Incidence, DALYs, and death data were downloaded from the GBD database and disaggregated by age, gender, and cause. R programming version 4.4.0 was utilized to visualize the data, determine temporal trends, and calculate percentage changes over the study period.
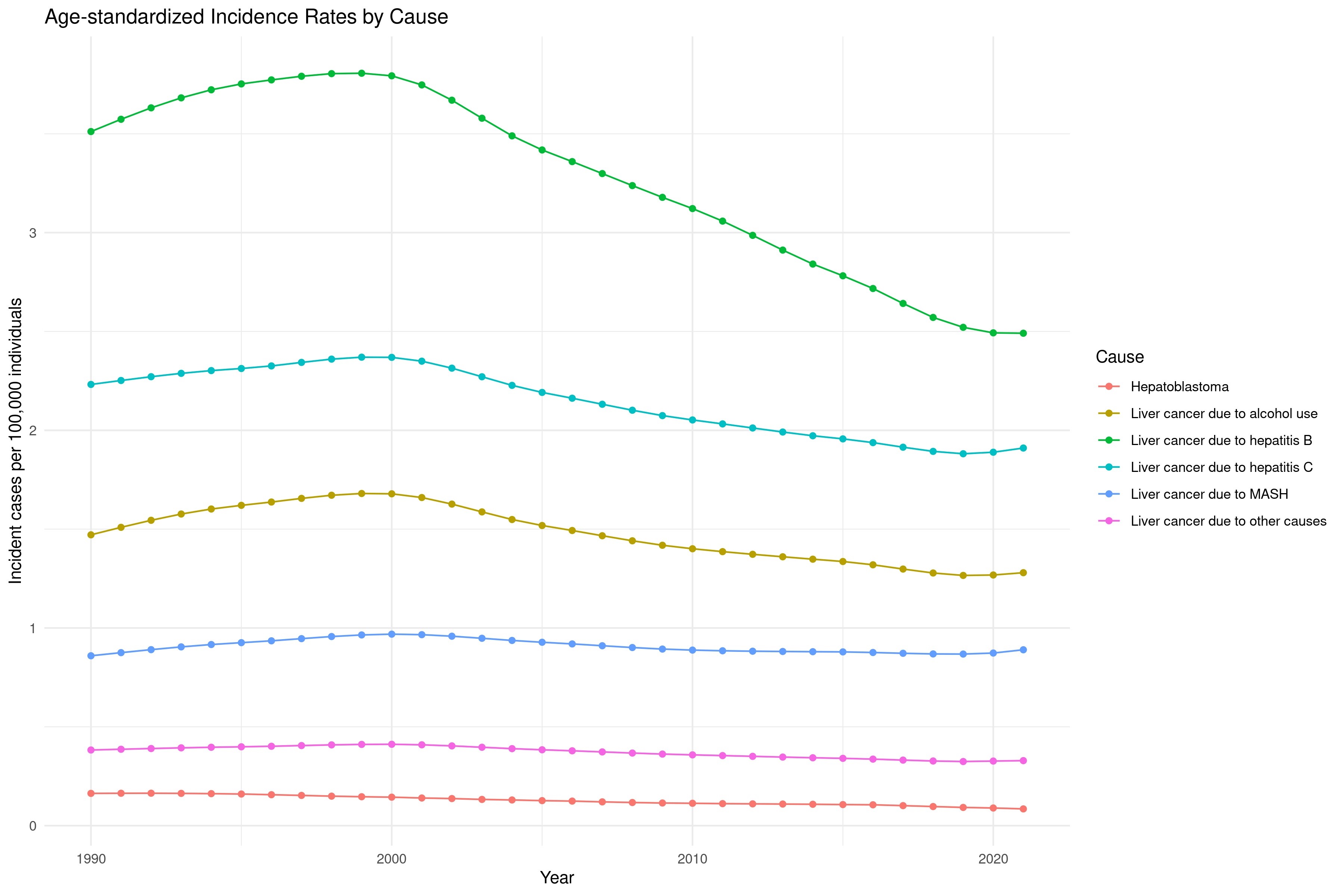
Results: The number of liver cancer cases in SSA increased from 20,237 in 1990 (95% CI: 14,183 - 28,104) to 36,186 in 2021 (95% CI: 29,785 - 44,727). Despite this increase, the age-standardized incidence rate per 100,000 decreased by 19.05%, from 8.62 (95% CI: 6.01 - 12.14) to 6.98 (95% CI: 5.84 - 8.48). Age-standardized death rates decreased by 18.10%, from 9.17 (95% CI: 6.41 - 12.97) to 7.51 (95% CI: 6.29 - 9.13), and DALYs decreased by 21.73%, from 253.55 (95% CI: 176.89 - 355.06) to 198.43 per 100,000 (95% CI: 163.14 - 246.47). Liver cancer due to hepatitis B remained the highest cause of cases from 1990 to 2021. All causes showed decreased incidence rates except for liver cancer secondary to metabolic-associated steatohepatitis (MASH), which increased by 3.49%, from 0.86 (95% CI: 0.53 - 1.33) to 0.89 (95% CI: 0.66 - 1.17).
Discussion: Significant progress has been achieved in reducing liver cancer incidence and mortality in SSA, primarily through vaccination programs and increased awareness of hepatitis C. These initiatives should be sustained and expanded. However, the rise in liver cancer cases due to MASH shows the necessity for targeted interventions. Additionally, a significant burden remains from other causes, many of which are modifiable risk factors. These findings show the need for continued, comprehensive public health strategies. Ensuring the prevention and management of all liver cancer risk factors is pivotal to further reducing the burden in the region.
Disclosures:
Omar Al Ta'ani, MD1, Yazan Al-Ajlouni, MD2, Yahya Alhalalmeh, MD3, Sharifeh Almasaid, MD4, Taimur S. Muzammil, MD5, Tyrell Daniel, MD5, Basile Njei, MD6. P2944 - The Burden of Liver Cancer in Sub-Saharan Africa: An Analysis From the Global Burden of Disease Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Allegheny Health Network, Pittsburgh, PA; 2Staten Island University Hospital, Northwell Health, New York, NY; 3New York Medical College - Saint Michael's Medical Center, Newark, NJ; 4SUNY Upstate Medical University, Johnson City, TN; 5Allegheny General Hospital, Pittsburgh, PA; 6Yale University School of Medicine, New Haven, CT
Introduction: Liver cancer poses a significant health burden in Sub-Saharan Africa (SSA), with some of the highest incidence and mortality rates globally. The region's high prevalence of hepatitis B and C, along with aflatoxin exposure and limited healthcare infrastructure, exacerbates the problem. Our study analyzes trends in liver cancer incidence, Disability-Adjusted Life Years (DALYs), and mortality in SSA from 1990 to 2021, providing insights to inform targeted interventions and policy decisions.
Methods: Data from the Global Burden of Disease (GBD) dataset were used to analyze the burden of liver cancer from 1990 to 2021. Incidence, DALYs, and death data were downloaded from the GBD database and disaggregated by age, gender, and cause. R programming version 4.4.0 was utilized to visualize the data, determine temporal trends, and calculate percentage changes over the study period.
Results: The number of liver cancer cases in SSA increased from 20,237 in 1990 (95% CI: 14,183 - 28,104) to 36,186 in 2021 (95% CI: 29,785 - 44,727). Despite this increase, the age-standardized incidence rate per 100,000 decreased by 19.05%, from 8.62 (95% CI: 6.01 - 12.14) to 6.98 (95% CI: 5.84 - 8.48). Age-standardized death rates decreased by 18.10%, from 9.17 (95% CI: 6.41 - 12.97) to 7.51 (95% CI: 6.29 - 9.13), and DALYs decreased by 21.73%, from 253.55 (95% CI: 176.89 - 355.06) to 198.43 per 100,000 (95% CI: 163.14 - 246.47). Liver cancer due to hepatitis B remained the highest cause of cases from 1990 to 2021. All causes showed decreased incidence rates except for liver cancer secondary to metabolic-associated steatohepatitis (MASH), which increased by 3.49%, from 0.86 (95% CI: 0.53 - 1.33) to 0.89 (95% CI: 0.66 - 1.17).
Discussion: Significant progress has been achieved in reducing liver cancer incidence and mortality in SSA, primarily through vaccination programs and increased awareness of hepatitis C. These initiatives should be sustained and expanded. However, the rise in liver cancer cases due to MASH shows the necessity for targeted interventions. Additionally, a significant burden remains from other causes, many of which are modifiable risk factors. These findings show the need for continued, comprehensive public health strategies. Ensuring the prevention and management of all liver cancer risk factors is pivotal to further reducing the burden in the region.
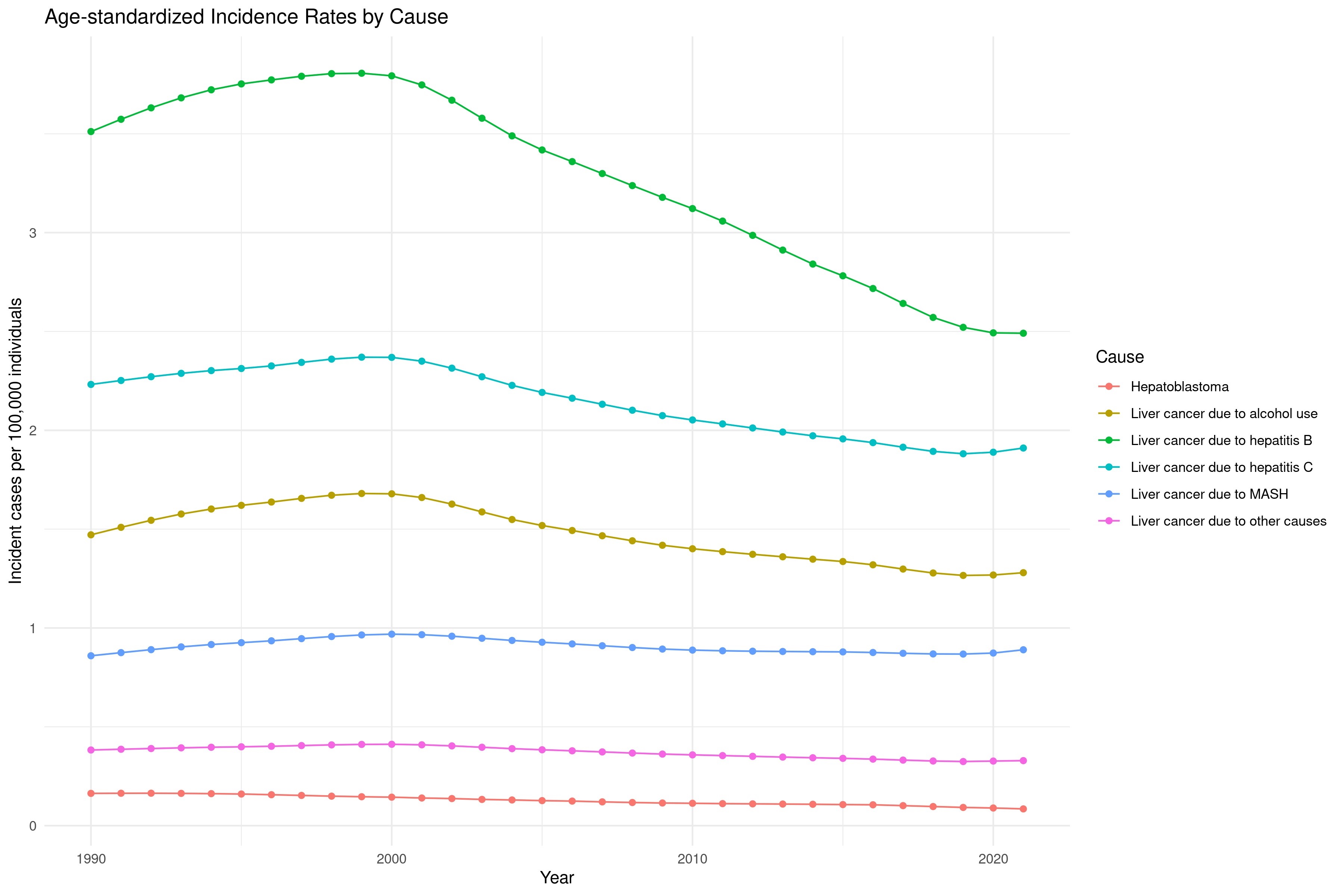
Figure: Trends in causes of incident cases of liver cancer from 1990-2021
Disclosures:
Omar Al Ta'ani indicated no relevant financial relationships.
Yazan Al-Ajlouni indicated no relevant financial relationships.
Yahya Alhalalmeh indicated no relevant financial relationships.
Sharifeh Almasaid indicated no relevant financial relationships.
Taimur Muzammil indicated no relevant financial relationships.
Tyrell Daniel indicated no relevant financial relationships.
Basile Njei indicated no relevant financial relationships.
Omar Al Ta'ani, MD1, Yazan Al-Ajlouni, MD2, Yahya Alhalalmeh, MD3, Sharifeh Almasaid, MD4, Taimur S. Muzammil, MD5, Tyrell Daniel, MD5, Basile Njei, MD6. P2944 - The Burden of Liver Cancer in Sub-Saharan Africa: An Analysis From the Global Burden of Disease Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
