Monday Poster Session
Category: Liver
P2857 - Higher Rate of SBP Recurrence With Secondary SBP Prophylaxis Compared to SBP Patients With Not on Prophylaxis in a National Cirrhosis Cohort
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- JB
Jasmohan S. Bajaj, MD
Virginia Commonwealth University and Central Virginia Veterans Healthcare System
Richmond, VA
Presenting Author(s)
Scott Silvey, MS1, Richard Sterling, MD2, Evan French, MS1, Nilang Patel, MD3, Jasmohan S.. Bajaj, MD4
1Virginia Commonwealth University, Richmond, VA; 2Virginia Commonwealth University Health System, Richmond, VA; 3Richmond VA Medical Center, Richmond, VA; 4Virginia Commonwealth University and Central Virginia Veterans Healthcare System, Richmond, VA
Introduction: Secondary prophylaxis with antibiotics is considered effective to prevent spontaneous bacterial peritonitis (SBP) recurrence. However, with greater resistance & gram-positive organisms, the effectiveness needs re-evaluation.
Methods: Using the TriNetX database, we created a cohort of pts with their first (index) SBP using validated ICD codes between 2009-2019. Patients were observed starting 30 days post-SBP for 2 years. Those who died or got a liver transplant (LT) during the same hospitalization as the SBP were excluded. Secondary prophylaxis was defined as continuous use of ciprofloxacin/Bactrim for ≥120 days post-SBP with ≥1 outpatient refill. Demographics, cirrhosis severity & admission medications were collected. SBP recurrence was defined as a new SBP episode ≥30 days post-index SBP. Those who died before recurrence were censored. Cox Proportional Hazards models were used to compare the rates of SBP recurrence adjusted for clinical differences. Interaction between SBP recurrence, index SBP year and SecSBPPr (2009-2011, 2012-2014, 2015-2017) was fit. Logistic regression models were also fit for all-cause mortality and LT rates during follow-up period.
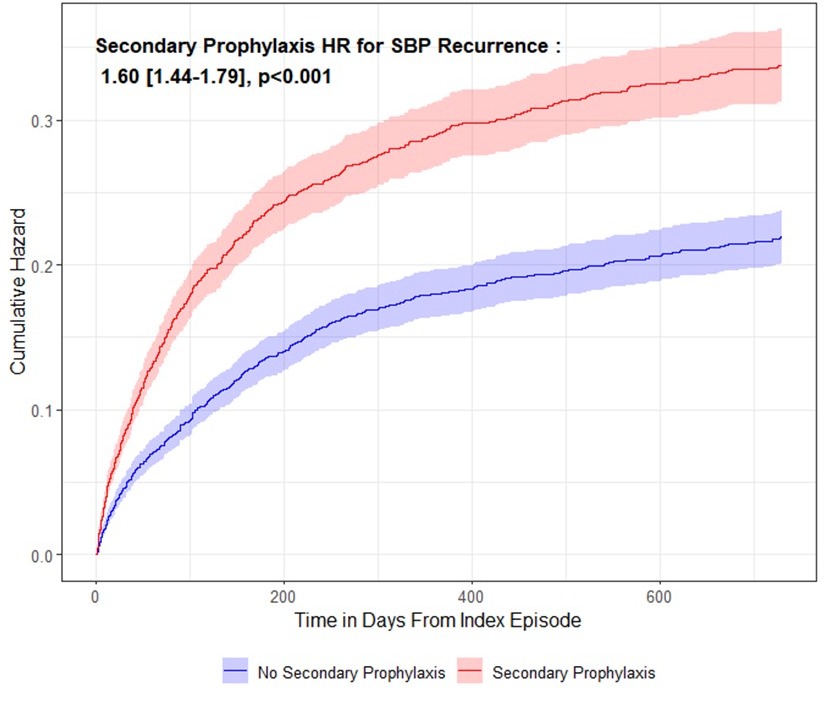
Results: 6754 patients with first SBP were included, of whom 3276 (48.5%) were on SecSBPPr. SecSBPPr pts were more likely to have prior complications and worse cirrhosis severity (Table 1). Univariable regression: SecSBPPr pts had higher rates of 2-year SBP recurrence (HR : 1.60 [1.44 –1.79], p< 0.001, Fig. 1), LT (OR : 2.87 [2.41–3.42], p< 0.001), and death (OR : 1.17 [1.06–1.29], p=0.002). Multivariable regression: After adjustment, the rate of 2-yr SBP recurrence remained significantly higher in SecSBPPr (1.56 [1.34-1.81], p< 0.001), as did the odds of liver transplant (2.64 [2.07-3.40], p< 0.001). Mortality was no longer statistically significant (p=0.973).
Multi-year interaction: SecSBPPr pts with index SBP 2012-2014 had 1.52× higher rates of recurrence vs those between 2009-2012 (p=0.077). This worsened with 2015-2017 patients who had 1.86× higher rates (p=0.004) for recurrence vs 2009-2012 pts.
Discussion: In a national cohort of cirrhosis patients after their first SBP episode, secondary SBP prophylaxis associates with a greater rate of SBP recurrence 2 years post-index episode versus those who were not given this prophylaxis even after adjusting for cirrhosis severity. Burden of SBP recurrence has worsened over time, likely due to higher resistance, which should prompt re-evaluation of this practice.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Scott Silvey, MS1, Richard Sterling, MD2, Evan French, MS1, Nilang Patel, MD3, Jasmohan S.. Bajaj, MD4. P2857 - Higher Rate of SBP Recurrence With Secondary SBP Prophylaxis Compared to SBP Patients With Not on Prophylaxis in a National Cirrhosis Cohort, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Virginia Commonwealth University, Richmond, VA; 2Virginia Commonwealth University Health System, Richmond, VA; 3Richmond VA Medical Center, Richmond, VA; 4Virginia Commonwealth University and Central Virginia Veterans Healthcare System, Richmond, VA
Introduction: Secondary prophylaxis with antibiotics is considered effective to prevent spontaneous bacterial peritonitis (SBP) recurrence. However, with greater resistance & gram-positive organisms, the effectiveness needs re-evaluation.
Methods: Using the TriNetX database, we created a cohort of pts with their first (index) SBP using validated ICD codes between 2009-2019. Patients were observed starting 30 days post-SBP for 2 years. Those who died or got a liver transplant (LT) during the same hospitalization as the SBP were excluded. Secondary prophylaxis was defined as continuous use of ciprofloxacin/Bactrim for ≥120 days post-SBP with ≥1 outpatient refill. Demographics, cirrhosis severity & admission medications were collected. SBP recurrence was defined as a new SBP episode ≥30 days post-index SBP. Those who died before recurrence were censored. Cox Proportional Hazards models were used to compare the rates of SBP recurrence adjusted for clinical differences. Interaction between SBP recurrence, index SBP year and SecSBPPr (2009-2011, 2012-2014, 2015-2017) was fit. Logistic regression models were also fit for all-cause mortality and LT rates during follow-up period.
Results: 6754 patients with first SBP were included, of whom 3276 (48.5%) were on SecSBPPr. SecSBPPr pts were more likely to have prior complications and worse cirrhosis severity (Table 1). Univariable regression: SecSBPPr pts had higher rates of 2-year SBP recurrence (HR : 1.60 [1.44 –1.79], p< 0.001, Fig. 1), LT (OR : 2.87 [2.41–3.42], p< 0.001), and death (OR : 1.17 [1.06–1.29], p=0.002). Multivariable regression: After adjustment, the rate of 2-yr SBP recurrence remained significantly higher in SecSBPPr (1.56 [1.34-1.81], p< 0.001), as did the odds of liver transplant (2.64 [2.07-3.40], p< 0.001). Mortality was no longer statistically significant (p=0.973).
Multi-year interaction: SecSBPPr pts with index SBP 2012-2014 had 1.52× higher rates of recurrence vs those between 2009-2012 (p=0.077). This worsened with 2015-2017 patients who had 1.86× higher rates (p=0.004) for recurrence vs 2009-2012 pts.
Discussion: In a national cohort of cirrhosis patients after their first SBP episode, secondary SBP prophylaxis associates with a greater rate of SBP recurrence 2 years post-index episode versus those who were not given this prophylaxis even after adjusting for cirrhosis severity. Burden of SBP recurrence has worsened over time, likely due to higher resistance, which should prompt re-evaluation of this practice.
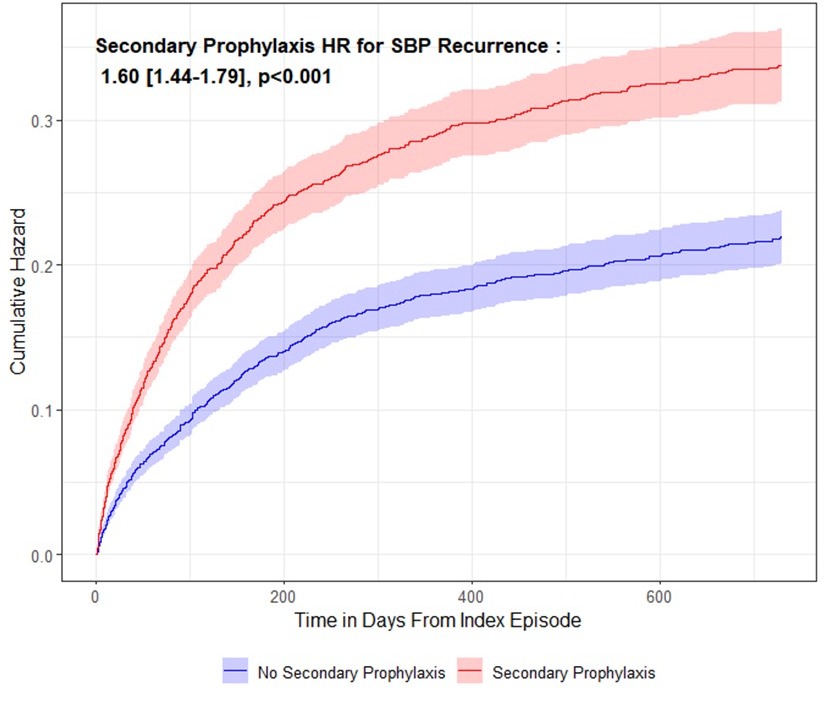
Figure: Figure 1 : Rates of SBP Recurrence During Follow-Up In Patients with SBP who were given Secondary Prophylaxis versus not
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Scott Silvey indicated no relevant financial relationships.
Richard Sterling indicated no relevant financial relationships.
Evan French indicated no relevant financial relationships.
Nilang Patel indicated no relevant financial relationships.
Jasmohan Bajaj: Salix Pharmaceuticals – Clinical Trial Investigator.
Scott Silvey, MS1, Richard Sterling, MD2, Evan French, MS1, Nilang Patel, MD3, Jasmohan S.. Bajaj, MD4. P2857 - Higher Rate of SBP Recurrence With Secondary SBP Prophylaxis Compared to SBP Patients With Not on Prophylaxis in a National Cirrhosis Cohort, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
