Monday Poster Session
Category: Liver
P2869 - Liver Decompensation and Mortality Outcomes Using Baveno VII Cutoffs for Transient Elastography Among Patients With Compensated Advanced Chronic Liver Disease in a Diverse, Urban US Cohort With Obesity and MASLD
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- Cm
Cyrus mowdawalla, MD
Montefiore Medical Center, Albert Einstein College of Medicine
Bronx, NY
Presenting Author(s)
Cyrus mowdawalla, MD1, Nina Kogekar, MD1, Joshua Wynne, MD1, S. Sharareh Dehghani, MD1, Vineela Nagamalla, MD1, Daniel Alvarez, MD2, Muhammad Khan, MD1, Garrick Luo, BS1, Ushna Awan, MD1, Zoe Verzani, BS1, Clara Y. Tow, MD1, Brett E. Fortune, MD, MS1
1Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 2Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, NY
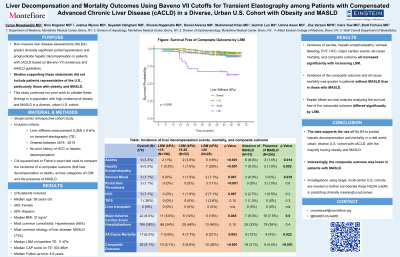
Introduction: Non-invasive liver disease assessments (NILDA), such as liver stiffness measurement (LSM) from transient elastography (TE), predict clinically significant portal hypertension and prognosticate hepatic decompensation among patients with compensated advanced chronic liver disease (cACLD) based on Baveno VII consensus and AASLD guidance on Portal Hypertension. Studies supporting these statements did not include patients representative of the U.S. This study continues our prior work to validate these findings in populations with high incidence of obesity andmetabolic dysfunction-associated steatotic liver disease (MASLD) in a diverse, urban U.S. cohort.
Methods: We conducted a single-center retrospective cohort study at an urban academic U.S. health system. Patients with LSM ≥ 8 kPa on TE performed in 2018 and 2019, with no prior history of hepatic decompensation or liver cancer, were included. Demographics, laboratory values, and clinical outcomes were recorded up to 5 years from baseline TE. Data were analyzed using R Version 4.3.0. Chi-squared test or Fisher’s exact test were used to compare the incidence of a composite outcome (first liver decompensation or death), across categories of LSM and the presence of MASLD.
Results: 276 patients with cACLD were included. The median age was 59 years (IQR: 51, 65), 58% were female, 58% were of Hispanic ethnicity, and median BMI was 31 kg/m2 (IQR: 27, 37). The most common etiology of liver disease was MASLD (73%). Median LSM on baseline TE was 11 kPa (IQR: 9, 16). Incidence of the composite outcome increased significantly with increasing LSM (5.1% in < 15 kPa, 9.6% in 15-25 kPa, 36% in >25 kPa; p < 0.001), and all-cause mortality (3.6% in < 15 kPa, 7.7% in 15-25 kPa, 21% in >25 kPa; p = 0.003). Incidence of the composite outcome was greater in patients without MASLD (21%) than in those with MASLD (4.5%; p < 0.001), as was incidence of mortality (12% without MASLD vs. 4% with MASLD, p = 0.022) (Table 1). Kaplan Meier survival analysis analyzing the survival free of the composite outcome differed significantly by LSM.
Discussion: We found increasing incidence of liver decompensation or mortality with increasing LSM on TE, supporting the use of NILDA to predict decompensation and mortality in a real-world, urban, diverse U.S. cohort with cACLD, and with the majority having obesity and MASLD. Investigations using larger, multi-center U.S. cohorts are needed to further corroborate these NILDA cutoffs in predicting clinically meaningful outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Cyrus mowdawalla, MD1, Nina Kogekar, MD1, Joshua Wynne, MD1, S. Sharareh Dehghani, MD1, Vineela Nagamalla, MD1, Daniel Alvarez, MD2, Muhammad Khan, MD1, Garrick Luo, BS1, Ushna Awan, MD1, Zoe Verzani, BS1, Clara Y. Tow, MD1, Brett E. Fortune, MD, MS1. P2869 - Liver Decompensation and Mortality Outcomes Using Baveno VII Cutoffs for Transient Elastography Among Patients With Compensated Advanced Chronic Liver Disease in a Diverse, Urban US Cohort With Obesity and MASLD, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 2Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, NY
Introduction: Non-invasive liver disease assessments (NILDA), such as liver stiffness measurement (LSM) from transient elastography (TE), predict clinically significant portal hypertension and prognosticate hepatic decompensation among patients with compensated advanced chronic liver disease (cACLD) based on Baveno VII consensus and AASLD guidance on Portal Hypertension. Studies supporting these statements did not include patients representative of the U.S. This study continues our prior work to validate these findings in populations with high incidence of obesity andmetabolic dysfunction-associated steatotic liver disease (MASLD) in a diverse, urban U.S. cohort.
Methods: We conducted a single-center retrospective cohort study at an urban academic U.S. health system. Patients with LSM ≥ 8 kPa on TE performed in 2018 and 2019, with no prior history of hepatic decompensation or liver cancer, were included. Demographics, laboratory values, and clinical outcomes were recorded up to 5 years from baseline TE. Data were analyzed using R Version 4.3.0. Chi-squared test or Fisher’s exact test were used to compare the incidence of a composite outcome (first liver decompensation or death), across categories of LSM and the presence of MASLD.
Results: 276 patients with cACLD were included. The median age was 59 years (IQR: 51, 65), 58% were female, 58% were of Hispanic ethnicity, and median BMI was 31 kg/m2 (IQR: 27, 37). The most common etiology of liver disease was MASLD (73%). Median LSM on baseline TE was 11 kPa (IQR: 9, 16). Incidence of the composite outcome increased significantly with increasing LSM (5.1% in < 15 kPa, 9.6% in 15-25 kPa, 36% in >25 kPa; p < 0.001), and all-cause mortality (3.6% in < 15 kPa, 7.7% in 15-25 kPa, 21% in >25 kPa; p = 0.003). Incidence of the composite outcome was greater in patients without MASLD (21%) than in those with MASLD (4.5%; p < 0.001), as was incidence of mortality (12% without MASLD vs. 4% with MASLD, p = 0.022) (Table 1). Kaplan Meier survival analysis analyzing the survival free of the composite outcome differed significantly by LSM.
Discussion: We found increasing incidence of liver decompensation or mortality with increasing LSM on TE, supporting the use of NILDA to predict decompensation and mortality in a real-world, urban, diverse U.S. cohort with cACLD, and with the majority having obesity and MASLD. Investigations using larger, multi-center U.S. cohorts are needed to further corroborate these NILDA cutoffs in predicting clinically meaningful outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Cyrus mowdawalla indicated no relevant financial relationships.
Nina Kogekar indicated no relevant financial relationships.
Joshua Wynne indicated no relevant financial relationships.
S. Sharareh Dehghani indicated no relevant financial relationships.
Vineela Nagamalla indicated no relevant financial relationships.
Daniel Alvarez indicated no relevant financial relationships.
Muhammad Khan indicated no relevant financial relationships.
Garrick Luo indicated no relevant financial relationships.
Ushna Awan indicated no relevant financial relationships.
Zoe Verzani indicated no relevant financial relationships.
Clara Tow indicated no relevant financial relationships.
Brett Fortune: BD Medical – Consultant. Cook Medical – Consultant. WL Gore and Associates – Consultant.
Cyrus mowdawalla, MD1, Nina Kogekar, MD1, Joshua Wynne, MD1, S. Sharareh Dehghani, MD1, Vineela Nagamalla, MD1, Daniel Alvarez, MD2, Muhammad Khan, MD1, Garrick Luo, BS1, Ushna Awan, MD1, Zoe Verzani, BS1, Clara Y. Tow, MD1, Brett E. Fortune, MD, MS1. P2869 - Liver Decompensation and Mortality Outcomes Using Baveno VII Cutoffs for Transient Elastography Among Patients With Compensated Advanced Chronic Liver Disease in a Diverse, Urban US Cohort With Obesity and MASLD, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

