Monday Poster Session
Category: Liver
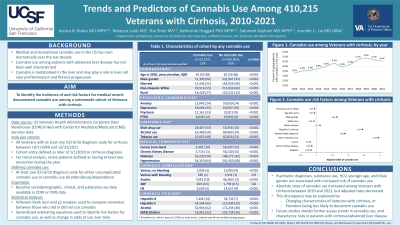
P2871 - Trends and Predictors of Cannabis Use Among 410,215 Veterans with Cirrhosis, 2010-2021
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JR
Jessica B. Rubin, MD, MPH
University of California San Francisco and San Francisco VA Health Care System
San Francisco, CA
Presenting Author(s)
Jessica B.. Rubin, MD, MPH1, Rebecca Loeb, MS2, Hui Shen, MS1, Katherine Hoggatt, PhD, MPH1, Salomeh Keyhani, MD, MPH1, Jennifer Lai, MD, MBA2
1University of California San Francisco and San Francisco VA Health Care System, San Francisco, CA; 2University of California San Francisco, San Francisco, CA
Introduction: Medical and recreational cannabis use in the US has risen drastically over the last decade among all demographics, but the incidence in those with advanced liver disease has not been well-characterized. We sought to identify the incidence of and risk factors for medical record-documented cannabis use among a nationwide cohort of Veterans with cirrhosis.
Methods: We used national data from the US Veterans Health Administration Corporate Data Warehouse and Center for Medicare/Medicaid Services to identify cannabis use among Veterans with cirrhosis 2010-2021. Cannabis use was defined as ³1 ICD-9 or 10 diagnosis code for cannabis use or cannabis use disorder/abuse/dependence. We used Wilcoxon Rank-Sum and χ2 analyses to compare demographic and clinical factors between those who did vs did not use cannabis. We used multivariable generalized estimating equation (GEE) regression models to identify risk factors for cannabis use, including a variable for the annual change in the odds of cannabis use.
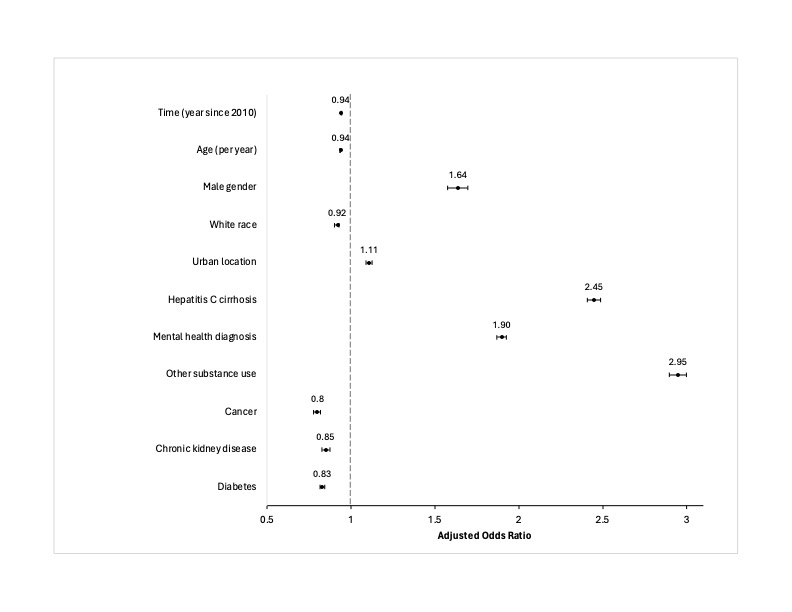
Results: Among 410,215 Veterans with cirrhosis, the overall rate of any documented cannabis use was 15%. The annual rate of documented cannabis use increased from 3% in 2010 to 5% in 2021. Cannabis users were younger, and more likely to be male, unmarried, non-White, and urban dwelling. Cannabis users had significantly higher rates of psychiatric comorbidities and other substance use, but lower rates of most other medical comorbidities (Table 1). On multivariable regression, Hepatitis C cirrhosis (vs all other cirrhosis etiologies) was associated with 2.5x the odds of cannabis use. After adjustment for cirrhosis etiology, as well as other demographic and clinical factors, the odds of documented cannabis use decreased each year during the study period (Figure 1).
Discussion: While absolute rates of cannabis use increased 2010-2021, adjusted rates decreased during this period. These findings suggest that either: (1) the absolute rise in cannabis use reflects changes in demographic and clinical makeup of Veterans with cirrhosis, or (2) that providers are becoming less likely to document cannabis use in the medical record as cannabis use in the US becomes increasingly common. In the setting of changing demographics of cirrhosis patients and increasing access to cannabis in the US, future studies should aim to further assess changes in cannabis use over time as well as the risks of cannabis in cirrhosis patients specifically.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jessica B.. Rubin, MD, MPH1, Rebecca Loeb, MS2, Hui Shen, MS1, Katherine Hoggatt, PhD, MPH1, Salomeh Keyhani, MD, MPH1, Jennifer Lai, MD, MBA2. P2871 - Trends and Predictors of Cannabis Use Among 410,215 Veterans with Cirrhosis, 2010-2021, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California San Francisco and San Francisco VA Health Care System, San Francisco, CA; 2University of California San Francisco, San Francisco, CA
Introduction: Medical and recreational cannabis use in the US has risen drastically over the last decade among all demographics, but the incidence in those with advanced liver disease has not been well-characterized. We sought to identify the incidence of and risk factors for medical record-documented cannabis use among a nationwide cohort of Veterans with cirrhosis.
Methods: We used national data from the US Veterans Health Administration Corporate Data Warehouse and Center for Medicare/Medicaid Services to identify cannabis use among Veterans with cirrhosis 2010-2021. Cannabis use was defined as ³1 ICD-9 or 10 diagnosis code for cannabis use or cannabis use disorder/abuse/dependence. We used Wilcoxon Rank-Sum and χ2 analyses to compare demographic and clinical factors between those who did vs did not use cannabis. We used multivariable generalized estimating equation (GEE) regression models to identify risk factors for cannabis use, including a variable for the annual change in the odds of cannabis use.
Results: Among 410,215 Veterans with cirrhosis, the overall rate of any documented cannabis use was 15%. The annual rate of documented cannabis use increased from 3% in 2010 to 5% in 2021. Cannabis users were younger, and more likely to be male, unmarried, non-White, and urban dwelling. Cannabis users had significantly higher rates of psychiatric comorbidities and other substance use, but lower rates of most other medical comorbidities (Table 1). On multivariable regression, Hepatitis C cirrhosis (vs all other cirrhosis etiologies) was associated with 2.5x the odds of cannabis use. After adjustment for cirrhosis etiology, as well as other demographic and clinical factors, the odds of documented cannabis use decreased each year during the study period (Figure 1).
Discussion: While absolute rates of cannabis use increased 2010-2021, adjusted rates decreased during this period. These findings suggest that either: (1) the absolute rise in cannabis use reflects changes in demographic and clinical makeup of Veterans with cirrhosis, or (2) that providers are becoming less likely to document cannabis use in the medical record as cannabis use in the US becomes increasingly common. In the setting of changing demographics of cirrhosis patients and increasing access to cannabis in the US, future studies should aim to further assess changes in cannabis use over time as well as the risks of cannabis in cirrhosis patients specifically.
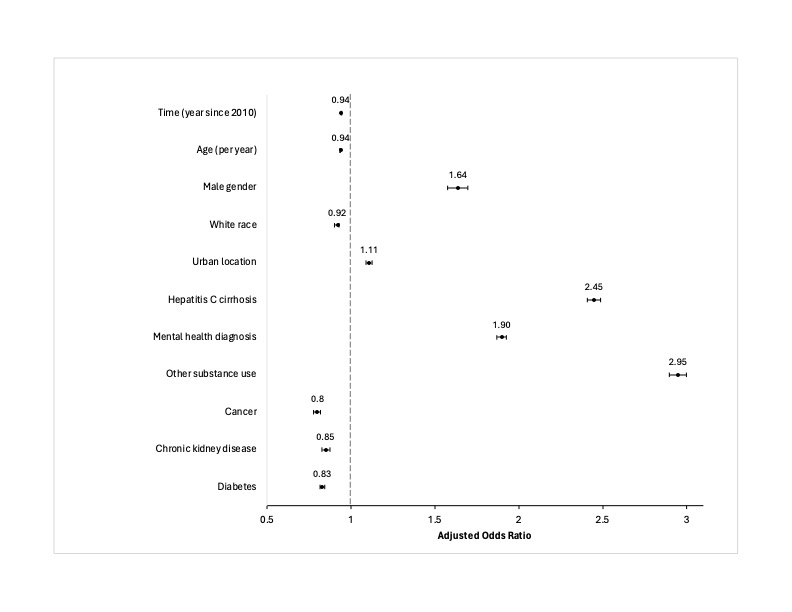
Figure: Figure 1. Multivariable generalized estimating equation model identifying risk factors for cannabis use
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jessica Rubin indicated no relevant financial relationships.
Rebecca Loeb indicated no relevant financial relationships.
Hui Shen indicated no relevant financial relationships.
Katherine Hoggatt indicated no relevant financial relationships.
Salomeh Keyhani indicated no relevant financial relationships.
Jennifer Lai: Boehringer Ingelheim – Consultant. Genfit – Consultant. Lipocene – Grant/Research Support. Nestle Nutrition Sciences – Grant/Research Support. Novo Nordisk – Advisory Committee/Board Member. Third Rock Ventures – Consultant. Vir Biotechnologies – Grant/Research Support.
Jessica B.. Rubin, MD, MPH1, Rebecca Loeb, MS2, Hui Shen, MS1, Katherine Hoggatt, PhD, MPH1, Salomeh Keyhani, MD, MPH1, Jennifer Lai, MD, MBA2. P2871 - Trends and Predictors of Cannabis Use Among 410,215 Veterans with Cirrhosis, 2010-2021, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
