Monday Poster Session
Category: Liver
P2872 - Trends in Secondary Liver Cancer-Related Mortality in the United States From 1999 to 2020
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Chun-Han Lo, MD, MPH
Kirk Kerkorian School of Medicine at the University of Nevada
Las Vegas, NV
Presenting Author(s)
Chun-Han Lo, MD, MPH1, Chun-Wei Pan, MD2, Rajan Amin, MD1, Vignan Manne, MD3
1Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, NV; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3Kirk Kirkorian School of Medicine, Las Vegas, NV
Introduction: Secondary liver cancers are more common than primary liver cancers. Mortality rates related to primary liver cancer have been rising. Less is known about mortality related to secondary liver cancer.
Methods: We conducted a cross-sectional study from 1999 to 2020 using the Multiple Cause of Death database from the Centers for Disease Control and Prevention’s (CDC) Wide-ranging Online Data for Epidemiologic Research (WONDER). We used ICD-10 codes to identify deaths related to secondary liver cancer and primary cancers among US residents. Age-adjusted mortality rates (AAMRs) were presented in deaths per 100,000 population. We obtained information on demographic characteristics from death certificates. Average annual percentage changes (AAPCs) were calculated using the Joinpoint regression program.
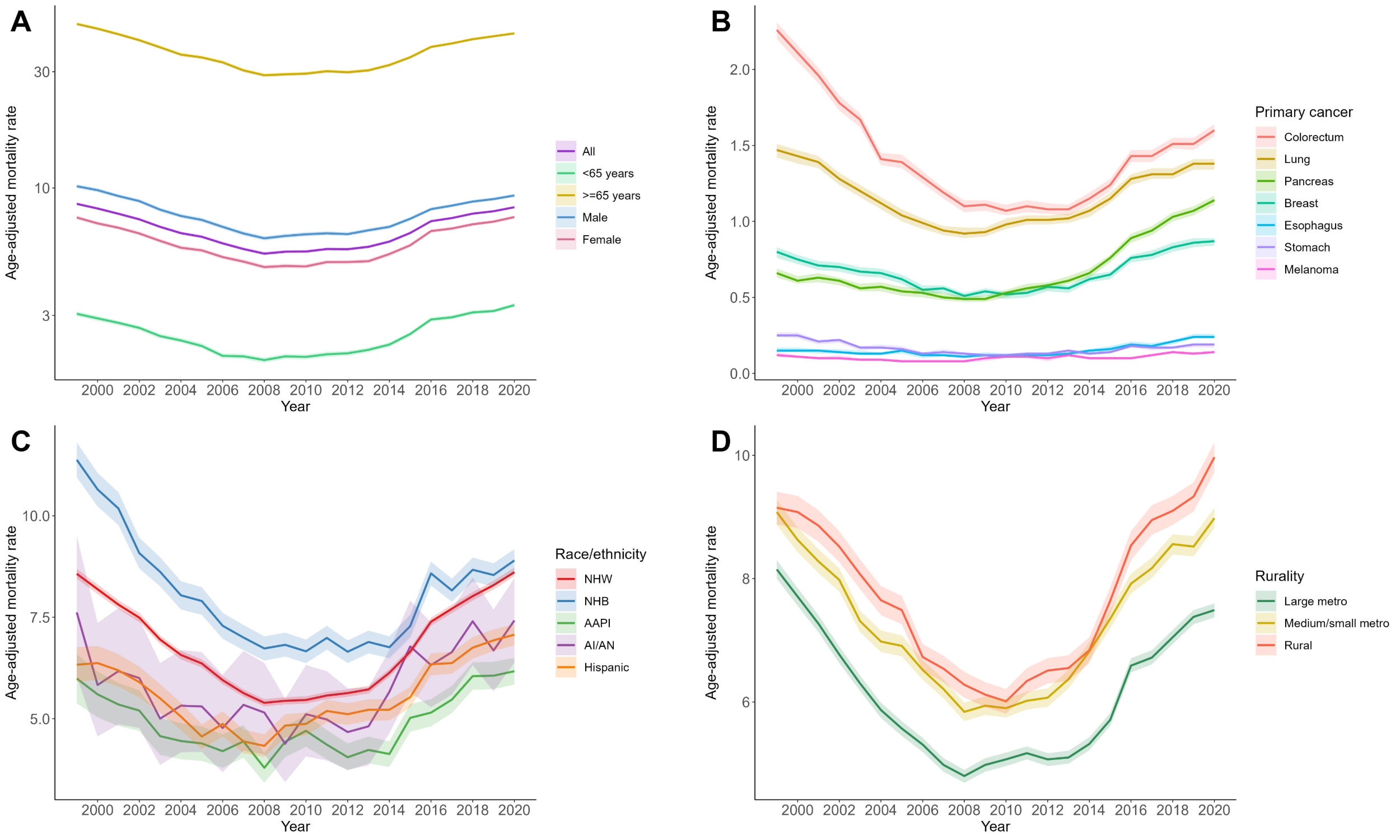
Results: Between 1999 and 2020, there were 503,145 deaths related to secondary liver cancer in 6,746,356,647 US residents (AAMR, 6.8; 95% CI, 6.7-6.8). AAMRs steadily declined from 8.6 (95% CI, 8.5-8.7) to 5.4 (95% CI, 5.3-5.5) between 1999 and 2008 (AAPC, -5.2%; 95% CI, -5.7% to -4.6%) but increased significantly to 8.3 (95% CI, 8.2-8.4) from 2008 to 2020 (AAPC, 3.8%; 95% CI, 3.2% to 4.1%) (Figure 1 & Table 1). Mortality related to metastatic pancreatic cancer, breast cancer, and esophageal cancer was greater in 2020 relative to 1999. The opposite pattern was seen in colorectal cancer and stomach cancer.
AAMRs were higher among older adults (36.1; 95% CI, 36.0-36.2) and males (7.8; 95%, 7.8-7.8) compared with their counterparts. Between racial/ethnic groups, AAMRs were highest in non-Hispanic Blacks (8.0; 95%, 8.0-8.1), followed by non-Hispanic Whites (6.8; 95%, 6.8-6.8), and lowest in Asian Americans and Pacific Islanders (5.0; 95% CI, 4.9-5.0). AAMRs were consistently greater in rural areas (7.7; 95% CI, 7.7-7.8) than in large metropolitan areas (6.1; 95% CI, 6.1-6.1).
Discussion: In the early 21st century, mortality related to secondary liver cancer demonstrated a U-shaped pattern. The initial decline can be explained by improved treatment and prevention of primary cancers. The latter trends are most likely attributable to increased diagnosis due to rising life expectancy and advancement in imaging technologies. The patterns of mortality changes differed by primary cancer. Absolute mortality rates differed by race/ethnicity and rurality. Efforts are needed to advance the care of secondary liver cancer and minimize disparities between populations.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Chun-Han Lo, MD, MPH1, Chun-Wei Pan, MD2, Rajan Amin, MD1, Vignan Manne, MD3. P2872 - Trends in Secondary Liver Cancer-Related Mortality in the United States From 1999 to 2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, NV; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3Kirk Kirkorian School of Medicine, Las Vegas, NV
Introduction: Secondary liver cancers are more common than primary liver cancers. Mortality rates related to primary liver cancer have been rising. Less is known about mortality related to secondary liver cancer.
Methods: We conducted a cross-sectional study from 1999 to 2020 using the Multiple Cause of Death database from the Centers for Disease Control and Prevention’s (CDC) Wide-ranging Online Data for Epidemiologic Research (WONDER). We used ICD-10 codes to identify deaths related to secondary liver cancer and primary cancers among US residents. Age-adjusted mortality rates (AAMRs) were presented in deaths per 100,000 population. We obtained information on demographic characteristics from death certificates. Average annual percentage changes (AAPCs) were calculated using the Joinpoint regression program.
Results: Between 1999 and 2020, there were 503,145 deaths related to secondary liver cancer in 6,746,356,647 US residents (AAMR, 6.8; 95% CI, 6.7-6.8). AAMRs steadily declined from 8.6 (95% CI, 8.5-8.7) to 5.4 (95% CI, 5.3-5.5) between 1999 and 2008 (AAPC, -5.2%; 95% CI, -5.7% to -4.6%) but increased significantly to 8.3 (95% CI, 8.2-8.4) from 2008 to 2020 (AAPC, 3.8%; 95% CI, 3.2% to 4.1%) (Figure 1 & Table 1). Mortality related to metastatic pancreatic cancer, breast cancer, and esophageal cancer was greater in 2020 relative to 1999. The opposite pattern was seen in colorectal cancer and stomach cancer.
AAMRs were higher among older adults (36.1; 95% CI, 36.0-36.2) and males (7.8; 95%, 7.8-7.8) compared with their counterparts. Between racial/ethnic groups, AAMRs were highest in non-Hispanic Blacks (8.0; 95%, 8.0-8.1), followed by non-Hispanic Whites (6.8; 95%, 6.8-6.8), and lowest in Asian Americans and Pacific Islanders (5.0; 95% CI, 4.9-5.0). AAMRs were consistently greater in rural areas (7.7; 95% CI, 7.7-7.8) than in large metropolitan areas (6.1; 95% CI, 6.1-6.1).
Discussion: In the early 21st century, mortality related to secondary liver cancer demonstrated a U-shaped pattern. The initial decline can be explained by improved treatment and prevention of primary cancers. The latter trends are most likely attributable to increased diagnosis due to rising life expectancy and advancement in imaging technologies. The patterns of mortality changes differed by primary cancer. Absolute mortality rates differed by race/ethnicity and rurality. Efforts are needed to advance the care of secondary liver cancer and minimize disparities between populations.
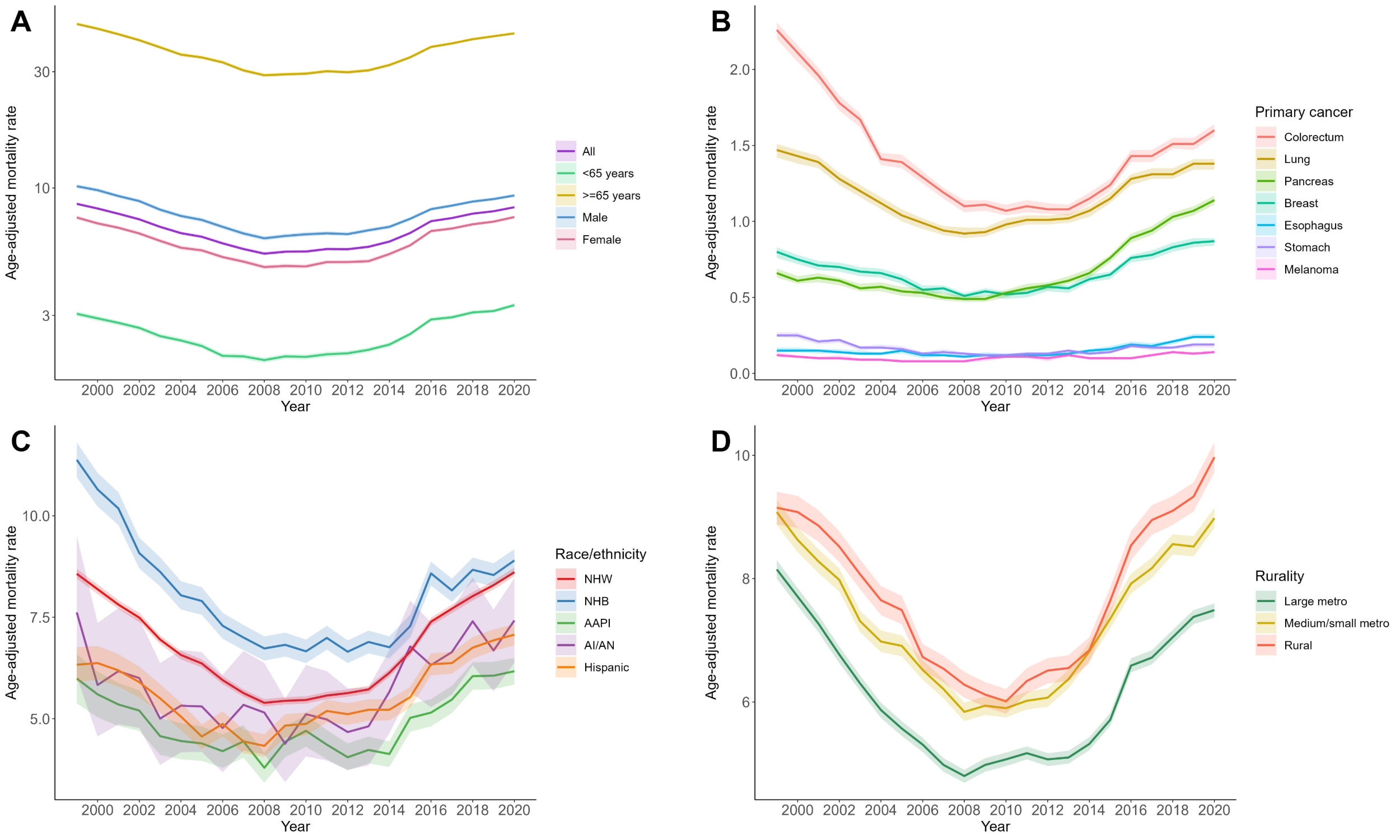
Figure: Figure 1. Trends in secondary liver cancer-related mortality in the US, 1999-2020. Age-adjusted mortality rates (AAMRs) were presented in deaths per 100,000 population. The shaded areas represent 95% confidence intervals. Abbreviations: AAPI, Asian American and Pacific Islander; AI/AN, American Indian and Alaska Native; NHB, non-Hispanic Black; NHW, non-Hispanic White.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Chun-Han Lo indicated no relevant financial relationships.
Chun-Wei Pan indicated no relevant financial relationships.
Rajan Amin indicated no relevant financial relationships.
Vignan Manne indicated no relevant financial relationships.
Chun-Han Lo, MD, MPH1, Chun-Wei Pan, MD2, Rajan Amin, MD1, Vignan Manne, MD3. P2872 - Trends in Secondary Liver Cancer-Related Mortality in the United States From 1999 to 2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
