Monday Poster Session
Category: Interventional Endoscopy
P2790 - Recovery and Functional Results Following Endoscopic Intramuscular Dissection for Invasive Rectal Carcinomas
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Kashif Ali, MD
University of Texas Rio Grande Valley
Edinburg, TX
Presenting Author(s)
Drumadala Gajbhiye, MBBS1, Kashif Ali, MD2, Azouba Gulraiz, MD3, Usama B. Shabbir, MD4, Muhammad Hassan Cheema, MD5, Muhammad Hussnain Cheema, MD5, Aeman Zafar, MBBS5, Noor Fatima, MBBS5, Alamdar Hussain, MD5, Humais H. Choudhary, MBBS6, Hamza Saleem, MD5, Ghulam Mustafa, MBBS7
1Government Medical College and Hospital, Akola, Maharashtra, India; 2University of Texas Rio Grande Valley, Edinburg, TX; 3Merit Health Wesley, Hattiesburg, MS; 4Services Institute of Medical Sciences, Lahore, Punjab, Pakistan; 5Nishtar Medical University, Multan, Punjab, Pakistan; 6Sahiwal Medical College, Sahiwal, Punjab, Pakistan; 7Dow University of Health Sciences, Karachi, Sindh, Pakistan
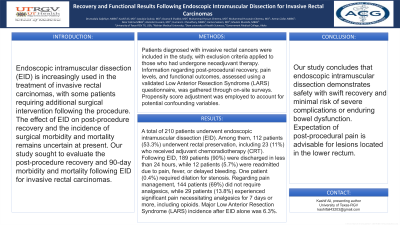
Introduction: Endoscopic intramuscular dissection (EID) is increasingly used in the treatment of invasive rectal carcinomas, with some patients requiring additional surgical intervention following the procedure. The effect of EID on post-procedure recovery and the incidence of surgical morbidity and mortality remains uncertain at present. Our study sought to evaluate the post-procedure recovery and 90-day morbidity and mortality following EID for invasive rectal carcinomas.
Methods: Patients diagnosed with invasive rectal cancers were included in the study, with exclusion criteria applied to those who had undergone neoadjuvant therapy. Information regarding post-procedural recovery, pain levels, and functional outcomes, assessed using a validated Low Anterior Resection Syndrome (LARS) questionnaire, was gathered through on-site surveys. Propensity score adjustment was employed to account for potential confounding variables.
Results: A total of 210 patients underwent endoscopic intramuscular dissection (EID). Among them, 112 patients (53.3%) underwent rectal preservation, including 23 (11%) who received adjuvant chemoradiotherapy (CRT). Following EID, 189 patients (90%) were discharged in less than 24 hours, while 12 patients (5.7%) were readmitted due to pain, fever, or delayed bleeding. One patient (0.4%) required dilation for stenosis. Regarding pain management, 144 patients (69%) did not require analgesics, while 29 patients (13.8%) experienced significant pain necessitating analgesics for 7 days or more, including opioids. Major Low Anterior Resection Syndrome (LARS) incidence after EID alone was 6.3%.
Discussion: Our study concludes that endoscopic intramuscular dissection demonstrates safety with swift recovery and minimal risk of severe complications or enduring bowel dysfunction. Expectation of post-procedural pain is advisable for lesions located in the lower rectum.
Disclosures:
Drumadala Gajbhiye, MBBS1, Kashif Ali, MD2, Azouba Gulraiz, MD3, Usama B. Shabbir, MD4, Muhammad Hassan Cheema, MD5, Muhammad Hussnain Cheema, MD5, Aeman Zafar, MBBS5, Noor Fatima, MBBS5, Alamdar Hussain, MD5, Humais H. Choudhary, MBBS6, Hamza Saleem, MD5, Ghulam Mustafa, MBBS7. P2790 - Recovery and Functional Results Following Endoscopic Intramuscular Dissection for Invasive Rectal Carcinomas, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Government Medical College and Hospital, Akola, Maharashtra, India; 2University of Texas Rio Grande Valley, Edinburg, TX; 3Merit Health Wesley, Hattiesburg, MS; 4Services Institute of Medical Sciences, Lahore, Punjab, Pakistan; 5Nishtar Medical University, Multan, Punjab, Pakistan; 6Sahiwal Medical College, Sahiwal, Punjab, Pakistan; 7Dow University of Health Sciences, Karachi, Sindh, Pakistan
Introduction: Endoscopic intramuscular dissection (EID) is increasingly used in the treatment of invasive rectal carcinomas, with some patients requiring additional surgical intervention following the procedure. The effect of EID on post-procedure recovery and the incidence of surgical morbidity and mortality remains uncertain at present. Our study sought to evaluate the post-procedure recovery and 90-day morbidity and mortality following EID for invasive rectal carcinomas.
Methods: Patients diagnosed with invasive rectal cancers were included in the study, with exclusion criteria applied to those who had undergone neoadjuvant therapy. Information regarding post-procedural recovery, pain levels, and functional outcomes, assessed using a validated Low Anterior Resection Syndrome (LARS) questionnaire, was gathered through on-site surveys. Propensity score adjustment was employed to account for potential confounding variables.
Results: A total of 210 patients underwent endoscopic intramuscular dissection (EID). Among them, 112 patients (53.3%) underwent rectal preservation, including 23 (11%) who received adjuvant chemoradiotherapy (CRT). Following EID, 189 patients (90%) were discharged in less than 24 hours, while 12 patients (5.7%) were readmitted due to pain, fever, or delayed bleeding. One patient (0.4%) required dilation for stenosis. Regarding pain management, 144 patients (69%) did not require analgesics, while 29 patients (13.8%) experienced significant pain necessitating analgesics for 7 days or more, including opioids. Major Low Anterior Resection Syndrome (LARS) incidence after EID alone was 6.3%.
Discussion: Our study concludes that endoscopic intramuscular dissection demonstrates safety with swift recovery and minimal risk of severe complications or enduring bowel dysfunction. Expectation of post-procedural pain is advisable for lesions located in the lower rectum.
Disclosures:
Drumadala Gajbhiye indicated no relevant financial relationships.
Kashif Ali indicated no relevant financial relationships.
Azouba Gulraiz indicated no relevant financial relationships.
Usama Shabbir indicated no relevant financial relationships.
Muhammad Hassan Cheema indicated no relevant financial relationships.
Muhammad Hussnain Cheema indicated no relevant financial relationships.
Aeman Zafar indicated no relevant financial relationships.
Noor Fatima indicated no relevant financial relationships.
Alamdar Hussain indicated no relevant financial relationships.
Humais Choudhary indicated no relevant financial relationships.
Hamza Saleem indicated no relevant financial relationships.
Ghulam Mustafa indicated no relevant financial relationships.
Drumadala Gajbhiye, MBBS1, Kashif Ali, MD2, Azouba Gulraiz, MD3, Usama B. Shabbir, MD4, Muhammad Hassan Cheema, MD5, Muhammad Hussnain Cheema, MD5, Aeman Zafar, MBBS5, Noor Fatima, MBBS5, Alamdar Hussain, MD5, Humais H. Choudhary, MBBS6, Hamza Saleem, MD5, Ghulam Mustafa, MBBS7. P2790 - Recovery and Functional Results Following Endoscopic Intramuscular Dissection for Invasive Rectal Carcinomas, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
