Monday Poster Session
Category: Interventional Endoscopy
P2804 - Malignancy-Related Ascites: The Role of Advanced Endoscopy for a Palliative Approach
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Maria Teresa Medina Rojas, MD
NYC Health + Hospitals/Jacobi
Brooklyn, NY
Presenting Author(s)
Maria Teresa Medina Rojas, MD1, Aarushi Sudan, MD2, Elias Estifan, MD3, Sammy Ho, MD, FACG3
1NYC Health + Hospitals/Jacobi, Brooklyn, NY; 2NYC Health + Hospitals/Jacobi, New York, NY; 3Montefiore Medical Center, New York, NY
Introduction: Recurrent malignant ascites impacts patients’ quality of life significantly. Although prognosis is generally poor, it is key to focus on providing relief from their symptoms. An intraluminal gastric stent can be offered as a palliative measure for appropriately selected patients. We present a case of a patient with loculated ascites causing gastric outlet obstruction.
Case Description/Methods: A 69-year-old Hispanic female with history of stage IIIC primary peritoneal carcinomatosis presented with abdominal pain, and PO intolerance. She had received neoadjuvant chemotherapy since diagnosis in 2022, debulking surgery followed by further chemotherapy, but her disease had been progressive with recurrent episodes of malignant ascites and partial small bowel obstruction.
Physical exam notable for for tachycardia to 117 bpm, uncomfortable-appearing female, distended abdomen and tender to palpation. Blood work noted pre-renal AKI (creatinine 3.6 mg/dL) and electrolyte derangements such as potassium 2.5mEq/L, phosphate was initially 6mg/dL, later decreased to 1.9 mg/dL. Supportive care was started such as IV fluids, electrolytes replacement, NGT placement but her symptoms did not improve.
CTAP showed multiple intraperitoneal loculated fluid collections increased in size with mass effect on the stomach. The gastroenterology service was consulted and recommended she undergo an endoscopic ultrasound which confirmed ascites measuring 10 cm. A lumen-apposing gastric stent was placed to drain her loculated ascites into her stomach. Her symptoms ameliorated within a week and repeat CTAP showed improvement in her ascitic collections, stent was removed. The patient was discharged home with close follow-up.
Discussion: Our patient’s presentation with abdominal pain, and emesis, was concerning for obstruction. Blood work showed pre-renal AKI, hypokalemia likely secondary to her PO intolerance. Supportive medical measures were unsuccessful. Imaging findings showed extrinsic compression of the stomach by ascitic collection. A lumen-apposing gastric stent was placed connecting the ascitic collection to the stomach. Symptomatology and imaging findings improved within a week and the gastric stent was removed. The patient was discharged home with close follow-up. In conclusion, advanced endoscopy provides a less invasive alternative to surgery in the care of our patients.

Disclosures:
Maria Teresa Medina Rojas, MD1, Aarushi Sudan, MD2, Elias Estifan, MD3, Sammy Ho, MD, FACG3. P2804 - Malignancy-Related Ascites: The Role of Advanced Endoscopy for a Palliative Approach, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYC Health + Hospitals/Jacobi, Brooklyn, NY; 2NYC Health + Hospitals/Jacobi, New York, NY; 3Montefiore Medical Center, New York, NY
Introduction: Recurrent malignant ascites impacts patients’ quality of life significantly. Although prognosis is generally poor, it is key to focus on providing relief from their symptoms. An intraluminal gastric stent can be offered as a palliative measure for appropriately selected patients. We present a case of a patient with loculated ascites causing gastric outlet obstruction.
Case Description/Methods: A 69-year-old Hispanic female with history of stage IIIC primary peritoneal carcinomatosis presented with abdominal pain, and PO intolerance. She had received neoadjuvant chemotherapy since diagnosis in 2022, debulking surgery followed by further chemotherapy, but her disease had been progressive with recurrent episodes of malignant ascites and partial small bowel obstruction.
Physical exam notable for for tachycardia to 117 bpm, uncomfortable-appearing female, distended abdomen and tender to palpation. Blood work noted pre-renal AKI (creatinine 3.6 mg/dL) and electrolyte derangements such as potassium 2.5mEq/L, phosphate was initially 6mg/dL, later decreased to 1.9 mg/dL. Supportive care was started such as IV fluids, electrolytes replacement, NGT placement but her symptoms did not improve.
CTAP showed multiple intraperitoneal loculated fluid collections increased in size with mass effect on the stomach. The gastroenterology service was consulted and recommended she undergo an endoscopic ultrasound which confirmed ascites measuring 10 cm. A lumen-apposing gastric stent was placed to drain her loculated ascites into her stomach. Her symptoms ameliorated within a week and repeat CTAP showed improvement in her ascitic collections, stent was removed. The patient was discharged home with close follow-up.
Discussion: Our patient’s presentation with abdominal pain, and emesis, was concerning for obstruction. Blood work showed pre-renal AKI, hypokalemia likely secondary to her PO intolerance. Supportive medical measures were unsuccessful. Imaging findings showed extrinsic compression of the stomach by ascitic collection. A lumen-apposing gastric stent was placed connecting the ascitic collection to the stomach. Symptomatology and imaging findings improved within a week and the gastric stent was removed. The patient was discharged home with close follow-up. In conclusion, advanced endoscopy provides a less invasive alternative to surgery in the care of our patients.

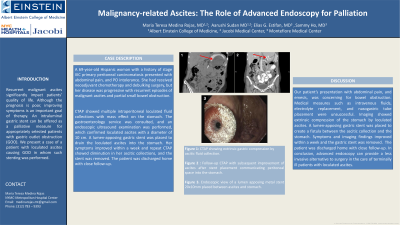
Figure: Figure 1: CTAP showing extrinsic gastric compression by ascitic fluid collection.
Figure 2: Follow-up CTAP with subsequent improvement after gastric metal stent was placed.
Figures 3 and 4: Endoscopic view of the lumen-apposing metal gastric stent 20x10mm on the day of the placement and on removal day, respectively.
Figure 2: Follow-up CTAP with subsequent improvement after gastric metal stent was placed.
Figures 3 and 4: Endoscopic view of the lumen-apposing metal gastric stent 20x10mm on the day of the placement and on removal day, respectively.
Disclosures:
Maria Teresa Medina Rojas indicated no relevant financial relationships.
Aarushi Sudan indicated no relevant financial relationships.
Elias Estifan indicated no relevant financial relationships.
Sammy Ho indicated no relevant financial relationships.
Maria Teresa Medina Rojas, MD1, Aarushi Sudan, MD2, Elias Estifan, MD3, Sammy Ho, MD, FACG3. P2804 - Malignancy-Related Ascites: The Role of Advanced Endoscopy for a Palliative Approach, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
