Monday Poster Session
Category: Interventional Endoscopy
P2809 - Endoscopic Rescue Mission: A Case Report Describing Eroded Lap Band Extraction
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Leilah A. Tisheh, MD
Long Island Community Hospital - NYU Langone Health System
Oceanside, NY
Presenting Author(s)
Leilah A. Tisheh, MD1, Sabrina Bulancea, MD2, Aanchal Tyagi, DO2, Prakash Viswanathan, MD, FACG2, Gloria Chu, MD2, Papiya Begum, MD2
1Long Island Community Hospital - NYU Langone Health System, Oceanside, NY; 2Long Island Community Hospital - NYU Langone Health System, Patchogue, NY
Introduction: Celebrated as a pioneering surgical innovation since its induction in 1993, laparoscopic implantation of an adjustable gastric band became one of the most common bariatric surgical operations in the world. An uncommon yet well-known complication involves erosion of the band through the gastric wall into the gastric lumen. The most common method of removal is done via laparoscopic approach however endoscopic removal is an alternative that is gaining favor. We describe a case of eroded lap band detection and subsequent endoscopic retrieval.
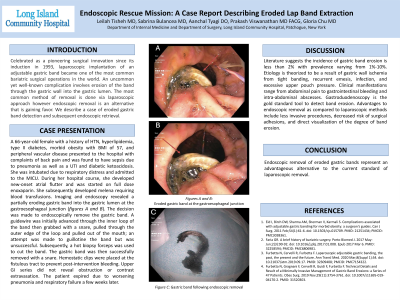
Case Description/Methods: A 66-year-old female with a history of HTN, HLD, type II diabetes, morbid obesity with BMI 57, PVD presented to the hospital with back pain and was found to have sepsis due to right lower lobe pneumonia and UTI with DKA. She was intubated for respiratory distress and admitted to MICU. During her hospital course, she developed new-onset atrial flutter and was started on full dose Lovenox. She developed melena requiring blood transfusions. Imaging and endoscopy revealed a partially eroding gastric band into the gastric lumen at the gastroesophageal junction. The decision was made to endoscopically remove the lap band. A guidewire was initially advanced through the inner loop of the band then grabbed with a snare, pulled through the outer edge of the loop and pulled out of the mouth and attempt was made to guillotine the band but was unsuccessful. Subsequently a hot biopsy forceps was used to cut the lap band. The lap band was then successfully removed with a snare. Hemostatic clips were placed at the fistulous tract to prevent post-intervention bleeding. Upper GI series did not reveal obstruction or contrast extravasation. The patient expired due to worsening pneumonia and respiratory failure a few weeks later.
Discussion: Literature suggests the incidence of lap band erosion is less than 2% with prevalence varying from 1%-10%. Etiology is theorized to be a result of gastric wall ischemia from tight banding, recurrent emesis, infection, and excessive upper pouch pressure. Clinical manifestations range from abdominal pain to GI bleeding and intra-abdominal abscesses. Gastroduodenoscopy is the gold standard diagnostic tool to detect band erosion. Advantages to endoscopic removal as compared to laparoscopic methods include less invasive procedures, decreased risk of surgical adhesions, and direct visualization of the degree of band erosion. Endoscopic removal of eroded lap bands represent an advantageous alternative to the current standard.

Disclosures:
Leilah A. Tisheh, MD1, Sabrina Bulancea, MD2, Aanchal Tyagi, DO2, Prakash Viswanathan, MD, FACG2, Gloria Chu, MD2, Papiya Begum, MD2. P2809 - Endoscopic Rescue Mission: A Case Report Describing Eroded Lap Band Extraction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Long Island Community Hospital - NYU Langone Health System, Oceanside, NY; 2Long Island Community Hospital - NYU Langone Health System, Patchogue, NY
Introduction: Celebrated as a pioneering surgical innovation since its induction in 1993, laparoscopic implantation of an adjustable gastric band became one of the most common bariatric surgical operations in the world. An uncommon yet well-known complication involves erosion of the band through the gastric wall into the gastric lumen. The most common method of removal is done via laparoscopic approach however endoscopic removal is an alternative that is gaining favor. We describe a case of eroded lap band detection and subsequent endoscopic retrieval.
Case Description/Methods: A 66-year-old female with a history of HTN, HLD, type II diabetes, morbid obesity with BMI 57, PVD presented to the hospital with back pain and was found to have sepsis due to right lower lobe pneumonia and UTI with DKA. She was intubated for respiratory distress and admitted to MICU. During her hospital course, she developed new-onset atrial flutter and was started on full dose Lovenox. She developed melena requiring blood transfusions. Imaging and endoscopy revealed a partially eroding gastric band into the gastric lumen at the gastroesophageal junction. The decision was made to endoscopically remove the lap band. A guidewire was initially advanced through the inner loop of the band then grabbed with a snare, pulled through the outer edge of the loop and pulled out of the mouth and attempt was made to guillotine the band but was unsuccessful. Subsequently a hot biopsy forceps was used to cut the lap band. The lap band was then successfully removed with a snare. Hemostatic clips were placed at the fistulous tract to prevent post-intervention bleeding. Upper GI series did not reveal obstruction or contrast extravasation. The patient expired due to worsening pneumonia and respiratory failure a few weeks later.
Discussion: Literature suggests the incidence of lap band erosion is less than 2% with prevalence varying from 1%-10%. Etiology is theorized to be a result of gastric wall ischemia from tight banding, recurrent emesis, infection, and excessive upper pouch pressure. Clinical manifestations range from abdominal pain to GI bleeding and intra-abdominal abscesses. Gastroduodenoscopy is the gold standard diagnostic tool to detect band erosion. Advantages to endoscopic removal as compared to laparoscopic methods include less invasive procedures, decreased risk of surgical adhesions, and direct visualization of the degree of band erosion. Endoscopic removal of eroded lap bands represent an advantageous alternative to the current standard.

Figure: Eroded lap band at the gastroesophageal junction (images A and B) and following endoscopic removal (image C).
Disclosures:
Leilah Tisheh indicated no relevant financial relationships.
Sabrina Bulancea indicated no relevant financial relationships.
Aanchal Tyagi indicated no relevant financial relationships.
Prakash Viswanathan indicated no relevant financial relationships.
Gloria Chu indicated no relevant financial relationships.
Papiya Begum indicated no relevant financial relationships.
Leilah A. Tisheh, MD1, Sabrina Bulancea, MD2, Aanchal Tyagi, DO2, Prakash Viswanathan, MD, FACG2, Gloria Chu, MD2, Papiya Begum, MD2. P2809 - Endoscopic Rescue Mission: A Case Report Describing Eroded Lap Band Extraction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
