Monday Poster Session
Category: IBD
P2713 - Congestive Ischemic Colitis: A Rare Mimic of Inflammatory Bowel Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jeremy Polman, DO, MS, MBA
Lenox Hill Hospital, Northwell Health
New York, NY
Presenting Author(s)
Jeremy Polman, DO, MS, MBA1, Jakob Saidman, MD1, Lauren A. Lyssy, DO2, Isabel Roitman, NP, MBA1, Arun Swaminath, MD3
1Lenox Hill Hospital, Northwell Health, New York, NY; 2The University of Tennessee Health Science Center, Memphis, TN; 3Lenox Hill Hospital/Northwell Health, New York, NY
Introduction: Patients with inflammatory bowel disease (IBD) commonly present with abdominal pain, diarrhea, hematochezia, and inflammation or ulceration identified on endoscopy. However, these findings are not specific to IBD and lead to a broad differential diagnosis.
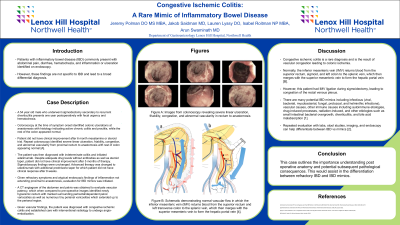
Case Description/Methods: A 54 year old male who underwent sigmoidectomy secondary to recurrent diverticulitis presents one year postoperatively with fecal urgency and hematochezia. Colonoscopy at the time of symptom onset identified colonic ulcerations at anastomosis with histology indicating active chronic colitis and proctitis, while the rest of the colon appeared normal. Patient did not have clinical improvement after 6 month mesalamine or steroid trial. Repeat colonoscopy identified severe linear ulceration, friability, congestion, and abnormal vascularity from proximal rectum to anastomosis with rest of colon appearing normal [A]. The patient was then diagnosed with indeterminate colitis and initiated adalimumab. Despite adequate drug levels without antibodies as well as steroid taper, patient did not have clinical improvement after 5 months of therapy. Sigmoidoscopy findings were unchanged. Advanced therapy was changed to ustekinumab with additional prednisone taper for which patient did not have clinical response after 8 weeks. Given refractory symptoms and atypical endoscopic findings of inflammation not extending proximal to anastomosis, evaluation for IBD mimics was initiated. A CT angiogram of the abdomen and pelvis was obtained to evaluate vascular patency, which when compared to pre-operative images identified newly hyperemic rectum with marked surrounding perirectal/dependent pelvic varicosities as well as numerous tiny perianal varicosities which extended up to the perianal region. Given vascular findings, the patient was diagnosed with congestive ischemic colitis and established care with interventional radiology to undergo angio-embolization.
Discussion: Congestive ischemic colitis is a rare diagnosis and is the result of vascular congestion leading to colonic ischemia. Normally, the inferior mesenteric vein (IMV) returns blood from the superior rectum, sigmoid, and left colon to the splenic vein, which then merges with the superior mesenteric vein to form the hepatic portal vein [B]. However, this patient had IMV ligation during sigmoidectomy, leading to congestion of the rectal venous plexus. This case outlines the importance of differentiation between refractory IBD and IBD mimics.

Disclosures:
Jeremy Polman, DO, MS, MBA1, Jakob Saidman, MD1, Lauren A. Lyssy, DO2, Isabel Roitman, NP, MBA1, Arun Swaminath, MD3. P2713 - Congestive Ischemic Colitis: A Rare Mimic of Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Lenox Hill Hospital, Northwell Health, New York, NY; 2The University of Tennessee Health Science Center, Memphis, TN; 3Lenox Hill Hospital/Northwell Health, New York, NY
Introduction: Patients with inflammatory bowel disease (IBD) commonly present with abdominal pain, diarrhea, hematochezia, and inflammation or ulceration identified on endoscopy. However, these findings are not specific to IBD and lead to a broad differential diagnosis.
Case Description/Methods: A 54 year old male who underwent sigmoidectomy secondary to recurrent diverticulitis presents one year postoperatively with fecal urgency and hematochezia. Colonoscopy at the time of symptom onset identified colonic ulcerations at anastomosis with histology indicating active chronic colitis and proctitis, while the rest of the colon appeared normal. Patient did not have clinical improvement after 6 month mesalamine or steroid trial. Repeat colonoscopy identified severe linear ulceration, friability, congestion, and abnormal vascularity from proximal rectum to anastomosis with rest of colon appearing normal [A]. The patient was then diagnosed with indeterminate colitis and initiated adalimumab. Despite adequate drug levels without antibodies as well as steroid taper, patient did not have clinical improvement after 5 months of therapy. Sigmoidoscopy findings were unchanged. Advanced therapy was changed to ustekinumab with additional prednisone taper for which patient did not have clinical response after 8 weeks. Given refractory symptoms and atypical endoscopic findings of inflammation not extending proximal to anastomosis, evaluation for IBD mimics was initiated. A CT angiogram of the abdomen and pelvis was obtained to evaluate vascular patency, which when compared to pre-operative images identified newly hyperemic rectum with marked surrounding perirectal/dependent pelvic varicosities as well as numerous tiny perianal varicosities which extended up to the perianal region. Given vascular findings, the patient was diagnosed with congestive ischemic colitis and established care with interventional radiology to undergo angio-embolization.
Discussion: Congestive ischemic colitis is a rare diagnosis and is the result of vascular congestion leading to colonic ischemia. Normally, the inferior mesenteric vein (IMV) returns blood from the superior rectum, sigmoid, and left colon to the splenic vein, which then merges with the superior mesenteric vein to form the hepatic portal vein [B]. However, this patient had IMV ligation during sigmoidectomy, leading to congestion of the rectal venous plexus. This case outlines the importance of differentiation between refractory IBD and IBD mimics.

Figure: Images from colonoscopy revealing severe linear ulceration, friability, congestion, and abnormal vascularity in rectum to anastomosis with colon distal to anastomosis appearing normal.
Disclosures:
Jeremy Polman indicated no relevant financial relationships.
Jakob Saidman indicated no relevant financial relationships.
Lauren Lyssy indicated no relevant financial relationships.
Isabel Roitman indicated no relevant financial relationships.
Arun Swaminath: abbvie – Grant/Research Support. janssen – Grant/Research Support.
Jeremy Polman, DO, MS, MBA1, Jakob Saidman, MD1, Lauren A. Lyssy, DO2, Isabel Roitman, NP, MBA1, Arun Swaminath, MD3. P2713 - Congestive Ischemic Colitis: A Rare Mimic of Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

